
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Heal Avascular Necrosis W/out Surgery?
Heal Avascular Necrosis W/out Surgery?
“Glucocorticoid- induced osteonecrosis develops in 9–40% of patients receiving long-term therapy although it may also occur with short-term exposure to high doses…As a result, osteonecrosis is the most common glucocorticoid-related complication associated with successful litigation [13].”
I think I have glucocorticoids-induced avascular necrosis but I have not been formally diagnosed with it. I believe I have this bone condition because of persistent shoulder pain as well as previous high-dose dexamethasone use. High-dose dexamethasone is the frequent companion of the chemotherapy regimens multiple myeloma patients and survivors undergo to treat their blood cancer.
My challenge is to heal or at least manage my bone disease. And I need to do this without conventional medicines. Well, let’s say I will work hard to figure our how to heal or just manage my avascular necrosis.
Possible therapies include:
- Acupunture
- Laser Acupuncture-
- Hyperbaric Oxygen Therapy
- Stem Cell Therapy (see below)
- Sonic Wave Therapy
For information about avascular necrosis, scroll down the page, post a question or comment and I will reply to you ASAP.
Thanks,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Lytic Lesions, Bone Health and Multiple Myeloma-
- Avascular Necrosis in the long-term Multiple Myeloma Survivor
- Steroid-Induced Shoulder Avascular, Osteonecrosis: I.D. Therapies
Glucocorticoid-induced osteonecrosis
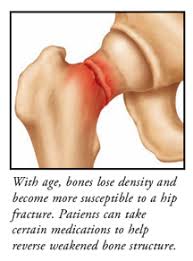
“Awareness of the need for prevention of glucocorticoid- induced fractures is growing, but glucocorticoid administration is often overlooked as the most common cause of nontraumatic osteonecrosis.
Glucocorticoid- induced osteonecrosis develops in 9–40% of patients receiving long-term therapy although it may also occur with short-term exposure to high doses, after intra-articular injection, and without glucocorticoid-induced osteoporosis…
Glucocorticoid-induced osteocyte apoptosis, a cumulative and unrepairable defect, uniquely disrupts the mechanosensory function of the osteocyte–lacunar–canalicular system and thus starts the inexorable sequence of events leading to collapse of the femoral head…
The average interval between initiation of treatment and the first symptoms of hip pain was 33 months, but several cases of osteonecrosis were noted after only 3 months…
Sadly, patients are seldom warned about this complication or the need to see their doctor if they experience persistent joint pain and radiological surveillance for osteonecrosis in patients receiving high-dose glucocorticoids is restricted to research studies [12].
- As a result, osteonecrosis is the most common glucocorticoid-related complication associated with successful litigation [13]…
- Most commonly, the hip is involved but almost any bone can develop osteonecrosis…
- Dexamethasone causes more skeletal complications than prednisone [27].
Glucocorticoid-induced osteocyte apoptosis accumulates and can lead to osteonecrosis, even without osteoporosis.
Conclusions- Glucocorticoids have direct adverse effects on osteoblasts, osteoclasts, and osteocytes. These drugs decrease lacunar– canalicular fluid, bone vascularity, and bone strength via their effects on osteocytes.
The risk of osteonecrosis increases with increasing dose and duration of treatment and dexamethasone may be the worst culprit. Alendronate may rapidly reduce pain, increase ambulation, and delay joint collapse in patients with osteonecrosis.”
[Acupotomy and acupuncture in the treatment of avascular necrosis of femoral head at the early and middle stages:a clinical randomized controlled trial]
“Objective: To compare the efficacy difference between acupotomy and acupuncture in the treatment of avascular necrosis of femoral head at the early and middle stages…
Results: Harris hip score was improved significantly after treatment in the two groups (both P<0.05). The result in acupotomy group was better than that in the acupuncture group (P<0.05). The effective rate was 90.6% (29/32) in the acupotomy group, better than 75.0% (21/28) in the acupuncture group after treatment (P<0.05).
Conclusions: Harris hip score and the effective rate in the acupotomy group are better than those in the treatment with routine acupuncture for avascular necrosis of femoral head at the early and middle stages.
Retrospective Study on Implantation of Autologous-Cultured Osteoblasts for the Treatment of Patients with Avascular Necrosis of the Femoral Head
“Purpose: Osteonecrosis of the femoral head is a progressive and debilitating disease that causes pain, osteoarthritis and hip joint collapse, eventually necessitating hip replacement. This study evaluated the long-term outcomes of autologous adult live-cultured osteoblasts (AALCO) implantation in patients with osteonecrosis of femoral head.
Patients and Methods: In this retrospective multicenter study, we collated and analyzed data of patients ≥ 12 years of age who underwent AALCO (OSSGROW®) between 2010 and 2015 for the treatment of osteonecrosis of the femoral head.
Results: Data from 64 patients (101 hip joints) were assessed in this study. The mean ±SD duration of disease since diagnosis of osteonecrosis was 7.4± 1.6 years. The mean follow-up duration was 6.3± 1.4 years. The mean VAS score (n=98 hips) reduced significantly from 58.8 ± 13.8 to 32.2 ± 32.1 post-operatively (mean difference: − 26.5± 35.2, p=0.001) and Harris hip score (n=97 hips) also significantly improved from 47.1± 12.3 to 63.7± 27.7 post-operatively (mean difference:16.7± 28.7, p=0.0001).
Following the AALCO treatment, 29 hips in 13 patients (28.7%) underwent total hip replacement (THA), indicating that AALCO treatment could delay THA for 71.3% of hips. A total of 39.1% of hips diagnosed in early stage versus 60.8% in the late stage of osteonecrosis required THA.
Overall, 60.4% of hips improved, 2% remained stable, and 37.6% progressed following the AALCO implantation. The condition of disease was found to have improved in 71.1% of patients in early stage (Grades I and II) versus 58% in the late stage (Grades III and IV) of osteonecrosis.
Conclusion: Patients with osteonecrosis who received implantation of autologous-cultured osteoblasts using AALCO showed improvement in joint function and decrease in pain. Treatment with AALCO halted progression of osteonecrosis, preserved the natural hip, and eliminated the need for hip replacement surgeries in 7 out of 10 patients.”
Avoiding hip replacement: How stem cells can treat avascular necrosis
“And that’s where stem cells come into play. Stem cells in our bone marrow can regenerate new blood vessels, muscle, and bone. “Because we’re able to replace injured bone with fresh bone, you may not need a more invasive procedure, such as a joint replacement,” Dr. Wiznia says…
For the procedure, Dr. Wiznia takes bone marrow from a patient’s pelvis and isolates the stem cells. He creates a 3D model of the patient’s hip joint so that he can precisely target the areas where bone is dead. He then removes some of the dead bone and injects stem cells—and places a bone graft—into those regions…”

