
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- non-conventional therapies »
- Adenocarcinoma Lung Cancer Stage 3B- Conventional and Non-Conventional?
Adenocarcinoma Lung Cancer Stage 3B- Conventional and Non-Conventional?
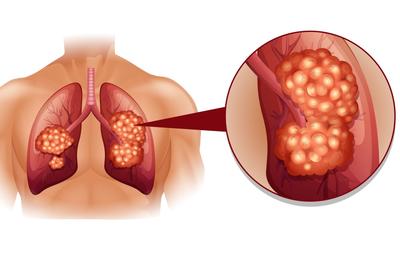
Pursue the Best of Both Conventional (FDA approved) and Non-Conventional Therapies to Manage Lung Cancer Effectively and Efficiently
Hi David- I am beside myself figuring out what to do next. Second opinion, alternative treatments, radiation and chemotherapy? I found you online and am asking for any help you could give me.
They say adenocarcinoma lung cancer stage 3B. I am going tomorrow for a brain scan and next week an ultrasound maxillary biosy. I have been going to Mercy Cancer Center in Merced, CA.
I have an appointment on the 22nd for a second opinion at Stanford Cancer Center in Palo Alto with a cancer panel and an appointment at Pacific/Orange Cancer Medical Center in Fresno on the 24th.
They are an alternative cancer center. Insurance doesn’t cover this one but was drawn to make an appointment anyway.
Thank you in advance for any information you can assist me with.
Hi Caroline-
- Consider antioxidants cited to cause apoptosis (kill) lung cancer-
- Consider supplementation shown to integrate or synergize with SOC chemotherapy
- Nutrition that either kills lung cancer or is anti-cancer
- Lifestyle therapies also that are are anti-cancer (whole-body hyperthermia, exercise, acupuncture, etc.)
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Lung Cancer and CT Scans-Are they worth it?
- Curcumin, Integrative Therapies, Can Overcome Multidrug-Resistance In Lung Cancer
- Metformin Improves Lung Cancer Survival by 66%
“Natural compounds such as curcumin have the ability to enhance the therapeutic effectiveness of common chemotherapy agents through cancer stem-like cell (CSC) sensitisation. In the present study, we showed that curcumin enhanced the sensitivity of the double-positive (CD166+/EpCAM+) CSC subpopulation in non-small cell lung cancer (NSCLC) cell lines (A549 and H2170) to cisplatin-induced apoptosis and inhibition of metastasis.
Our results revealed that initial exposure of NSCLC cell lines to curcumin (10-40 µM) markedly reduced the percentage of viability to an average of ~51 and ~54% compared to treatment with low dose cisplatin (3 µM) with only 94 and 86% in both the A549 and H2170 cells.
Moreover, sensitisation of NSCLC cell lines to curcumin through combined treatment enhanced the single effect induced by low dose cisplatin on the apoptosis of the double-positive CSC subpopulation by 18 and 20% in the A549 and H2170 cells, respectively.
Furthermore, we found that curcumin enhanced the inhibitory effects of cisplatin on the highly migratory CD166+/EpCAM+ subpopulation, marked by a reduction in cell migration to 9 and 21% in the A549 and H2170 cells, respectively, indicating that curcumin may increase the sensitivity of CSCs to cisplatin-induced migratory inhibition.
We also observed that the mRNA expression of cyclin D1 was downregulated, while a substantial increased in p21 expression was noted, followed by Apaf1 and caspase-9 activation in the double-positive (CD166+/EpCAM+) CSC subpopulation of A549 cells, suggested that the combined treatments induced cell cycle arrest, therefore triggering CSC growth inhibition via the intrinsic apoptotic pathway.
In conclusion, we provided novel evidence of the previously unknown therapeutic effects of curcumin, either alone or in combination with cisplatin on the inhibition of the CD166+/EpCAM+ subpopulation of NSCLC cell lines. This finding demonstrated the potential therapeutic approach of using curcumin that may enhance the effects of cisplatin by targeting the CSC subpopulation in NSCLC.”
Omega-3 Polyunsaturated Fatty Acids and Lung Cancer: nutrition or Pharmacology?
ω-3 PUFAs play essential roles in cell signaling and in cell structure and fluidity of membranes. They participate in the resolution of inflammation and have anti-inflammatory effects. Lung cancer patients suffer complications, such as anorexia-cachexia syndrome, pain and depression.
The European Society for Clinical Nutrition and Metabolism (ESPEN) 2017 guidelines for cancer patients only discuss the use of ω-3 PUFAs for cancer-cachexia treatment, leaving aside other cancer-related complications that could potentially be managed by ω-3 PUFAs.
This review aims to elucidate whether the effects of ω-3 PUFAs in lung cancer is supplementary, pharmacological or both. In addition, clinical studies, evidence in cell lines and animal models suggest how ω-3 PUFAs induce anticancer effects. ω-3 PUFAs and their metabolites are suggested to modulate pivotal pathways underlying the progression or complications of lung cancer, indicating that this is a promising field to be explored. Further investigation is still required to analyze the benefits of ω-3 PUFAs as supplementation or pharmacological treatment in lung cancer.”


