
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- Lung Cancer »
- Advanced Lung Cancer- Is Immunotherapy For You?
Advanced Lung Cancer- Is Immunotherapy For You?
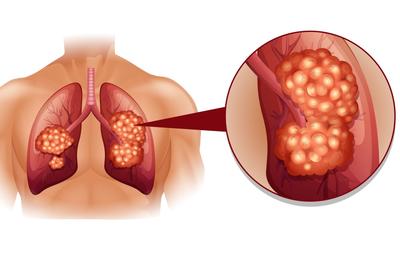
A Five-Year Survival Rate of 16% For Non-Small Cell Lung Cancer May Be Triple Previous Chemo Regimens but This is Hardly a Breakthrough…
Immunotherapy, “”treatment of disease by inducing, enhancing, or suppressing an immune response“ is supposed to be the future of cancer care. And while an immunotherapy such as Opdivo can be a useful therapy for advanced lung cancer patients, it’s important to understand that Opdivo is not curative.
And though Opdivo may cause fewer side effects, on average, than conventional chemotherapies, again, it is critical to consider evidence-based but non-conventional complementary, integrative and alternative therapies.
While immunotherapy may be an important advance for conventional oncology, complementary therapies such as probiotics may continue to offer an advantage to cancer patients and survivors.
I am a survivor of a completely different but “incurable” cancer called multiple myeloma. I have managed my cancer since my diagnosis in 1994 by living an evidence-based, non-toxic, anti-MM lifestyle through nutrition, supplementation, and many other therapies.
I am also a cancer coach. To learn more about evidence-based but non-toxic therapies to manage your advanced lung cancer scroll down the page, post a question or comment and I will reply to you ASAP.
Thank you,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Early Lung Cancer Therapies Reduce Cancer Deaths Significantly
- Early Lung Cancer, SBRT if Surgery is Not an Option
- The Cure for Lung Cancer May Be in Fish Oil
- Fish Oil Improves Response to Chemo, Improves OS for Lung Cancer Patients
Opdivo More Than Tripled 5-Year Survival Rates in NSCLC Patients in Phase 1 Study
“Recent data from a Phase 1 study revealed that Opdivo-treated advanced non-small cell lung cancer (NSCLC) patients have durable responses and a five-year survival rate of 16%, which more than triples the 4.9% five-year survival rate seen in historical controls receiving standard-of-care…
“This is the first report of the long-term survival rate in patients with metastatic NSCLC treated with an immune checkpoint inhibitor. Our study results show that for a small subset of patients, immunotherapy can work for a very long time…”
Among 10 responders evaluable for analysis, seven had PD-L1 expression of 1% or more, and three had PD-L1 expression lower than 1%. The presence of this ligand is usually used as a biomarker to predict which patients will respond to Opdivo, but in this study, PD-L1 status was not clearly associated with long-term survival in this patient population…”
Clinical impact of probiotics on the efficacy of anti-PD-1 monotherapy in patients with nonsmall cell lung cancer: A multicenter retrospective survival analysis study with inverse probability of treatment weighting
The gastrointestinal microbiota was reported as an important factor for the response to cancer immunotherapy. Probiotics associated with gastrointestinal dysbiosis and bacterial richness may affect the efficacy of cancer immunotherapy drugs.
However, the clinical impact of probiotics on the efficacy of cancer immunotherapy in patients with nonsmall cell lung cancer (NSCLC) is poorly understood. The outcomes of 294 patients with advanced or recurrent NSCLC who received antiprogrammed cell death-1 (PD-1) therapy (nivolumab or pembrolizumab monotherapy) at three medical centers in Japan were analyzed in our study.
We used inverse probability of treatment weighting (IPTW) to minimize the bias arising from the patients’ backgrounds. The IPTW-adjusted Kaplan-Meier curves showed that progression-free survival (nonuse vs use: hazard ratio [HR] [95% confidence interval {CI}] = 1.73 [1.42-2.11], log-rank test P = .0229), but not overall survival (nonuse vs use: HR [95%CI] = 1.40 [1.13-1.74], log-rank test P = .1835), was significantly longer in patients who received probiotics.
Moreover, the IPTW-adjusted univariate analyses showed that nonuse or use of probiotics was significantly associated with disease control (nonuse vs use: odds ratio [OR] [95%CI] = 0.51 [0.35-0.74], P = .0004) and overall response (nonuse vs use: OR [95%CI] = 0.43 [0.29-0.63], P < .0001).
In this multicenter and retrospective study, probiotics use was associated with favorable clinical outcomes in patients with advanced or recurrent NSCLC who received anti-PD-1 monotherapy. The findings should be validated in a future prospective study.”

