Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Overall Survival for RR/MM Patients
Overall Survival for RR/MM Patients

“The addition of isatuximab to pomalidomide-dexamethasone significantly improves progression-free survival in patients with relapsed, refractory multiple myeloma.”
What is “relapsed, refractory” and what does it mean for you?
You’ve been diagnosed with multiple myeloma, an incurable blood cancer. You were diagnosed and underwent the FDA approved standard-of-care treatment plan for newly diagnosed MM patients:
- Induction therapy (RVd or RVdD)
- With or W/out Autologous stem cell transplant (ASCT)
- Maintenance Chemotherapy
Your diagnostic testing indicated that you responded to your induction therapy but your numbers are trending up. You have relapsed and you are evaluating possible therapy plans.
I have good news and bad news.
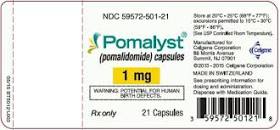
The good news is that a possible choice for you is outlined in the studies linked below. Pomalidomide (pomalyst), Isatuximab (sarclisa), dexamethasone (PId) has been shown to provide a longer PFS as well as a longer overall survival (OS) in MM. Importantly, this combo has been shown to work for MM patients who have already undergone both revlimid as well as velcade.
The not-so-good news is discussed below but I want to treat the issues fully.
PId can extend OS but this survival comes at a cost. PId is a lot of toxicity. The risk of side effects is high. To excerpt the study “serious treatment-emergent adverse events were observed in 111 (73%) patients in the isatuximab group.”
I would be remiss if I didn’t mention evidence-based but non-toxic therapies that may help you improve your health including:
- Detoxification
- Whole-body hyperthermia
- Anti-MM nutrition
and more.
If you are wondering about CAR-T therapy as a possible therapy option, yes it is. However, based on my research and mm feedback, CAR-T therapy also comes with serious side effects (inflammation), a coverage issues aka health care costs and finally, as of the writing of this post, CAR-T therapy doesn’t last long either.
I believe that CAR-T therapy offers a great deal of potential for the RR/MM patient. As of today, however, more work needs to be done on this therapy.
If you have any questions or comments, scroll down the page, post a question or a comment. I will reply to you ASAP.
Hang in there,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
The PeopleBeatingCancer Side Effects Program
New Combo May Set New Standard of Care for R/R MM
“Isatuximab plus pomalidomide and dexamethasone resulted in improved overall survival (OS) for patients with refractory or relapsed (R/R) multiple myeloma (MM) compared with pomalidomide and dexamethasone alone, and is a new standard of care for such patients, according to follow-up analysis from the phase 3 ICARIA-MM trial.
In the multicenter, open-label study, a total of 307 adult patients were randomized. Subjects had to have received at least 2 previous lines of therapy, including lenalidomide and a proteasome inhibitor, and had an Eastern Cooperative Oncology Group performance status of 0–2…
For purposes of the analysis, they were stratified by number of previous treatment lines (2–3 vs >3) to isatuximab–pomalidomide–dexamethasone (isatuximab group) or pomalidomide–dexamethasone (control group), and followed until disease progression, unacceptable toxicity, or withdrawal of consent.
The researchers conducted an updated overall survival (OS) analysis at 24 months after primary analysis. Participation in the treatment arm resulted in a 6.9-month difference in median OS:
- 24.6 months in the isatuximab group and
- 17.7 months in the control group respectively.
Serious treatment-emergent adverse events were observed in 111 (73%) patients in the isatuximab group and 90 (60%) patients in the control group. Median follow-up at data cutoff (Oct 1, 2020) was 35.3 months. Final overall survival follow-up analysis is ongoing…”
Isatuximab plus pomalidomide and low-dose dexamethasone versus pomalidomide and low-dose dexamethasone in patients with relapsed and refractory multiple myeloma (ICARIA-MM)
“Background: Isatuximab is a monoclonal antibody that binds a specific epitope on the human CD38 receptor and has antitumour activity via multiple mechanisms of action.
In a previous phase 1b study, around 65% of patients with relapsed and refractory multiple myeloma achieved an overall response with a combination of isatuximab with pomalidomide and low-dose dexamethasone.
The aim of this study was to determine the progression-free survival benefit of isatuximab plus pomalidomide and dexamethasone compared with pomalidomide and dexamethasone in patients with relapsed and refractory multiple myeloma.
Methods: We did a randomised, multicentre, open-label, phase 3 study at 102 hospitals in 24 countries in Europe, North America, and the Asia-Pacific regions. Eligible participants were adult patients with relapsed and refractory multiple myeloma who had received at least two previous lines of treatment, including lenalidomide and a proteasome inhibitor…
Both groups received oral pomalidomide on days 1 to 21 in each cycle, and oral or intravenous dexamethasone on days 1, 8, 15, and 22 of each cycle. Treatment continued until disease progression, unacceptable toxicity, or consent withdrawal.
Dose reductions for adverse reactions were permitted for pomalidomide and dexamethasone, but not for isatuximab. The primary endpoint was progression-free survival, determined by an independent response committee and assessed in the intention-to-treat population. Safety was assessed in all participants who received at least one dose of study drug. This study is registered at ClinicalTrials.gov, number NCT02990338.
Findings: Between Jan 10, 2017, and Feb 2, 2018, we randomly assigned 307 patients to treatment: 154 to isatuximab-pomalidomide-dexamethasone, and 153 to pomalidomide-dexamethasone.
At a median follow-up of 11·6 months (IQR 10·1-13·9), median progression-free survival was 11·5 months (95% CI 8·9-13·9) in the isatuximab-pomalidomide-dexamethasone group versus 6·5 months (4·5-8·3) in the pomalidomide-dexamethasone group; hazard ratio 0·596, 95% CI 0·44-0·81; p=0·001 by stratified log-rank test.
The most frequent treatment-emergent adverse events (any grade; isatuximab-pomalidomide-dexamethasone vs pomalidomide-dexamethasone) were
- infusion reactions (56 [38%] vs 0),
- upper respiratory tract infections (43 [28%] vs 26 [17%]), and
- diarrhoea (39 [26%] vs 29 [20%]).
Adverse events with a fatal outcome were reported in 12 patients (8%) in the isatuximab-pomalidomide-dexamethasone group and 14 (9%) in the pomalidomide-dexamethasone group.
Deaths due to treatment-related adverse events were reported for one patient (<1%) in the isatuximab-pomalidomide-dexamethasone group (sepsis) and two (1%) in the pomalidomide-dexamethasone group (pneumonia and urinary tract infection).
Interpretation: The addition of isatuximab to pomalidomide-dexamethasone significantly improves progression-free survival in patients with relapsed and refractory multiple myeloma. Isatuximab is an important new treatment option for the management of relapsed and refractory myeloma, particularly for patients who become refractory to lenalidomide and a proteasome inhibitor.”