Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- A-fib Stem Cell Transplant – Myeloma –
A-fib Stem Cell Transplant – Myeloma –

“Our data suggest that arrhythmia (A-fib) after transplants are associated with significant morbidity and mortality. A prospective study of arrhythmia in the transplant setting is warranted.”
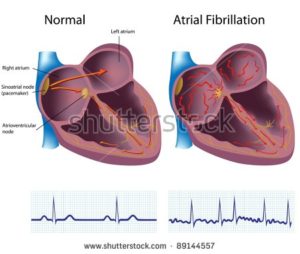
I was diagnosed with multiple myeloma in 2/94. I underwent an autologous stem cell transplant in 12/95. I developed chronic atrial fibrillation (A-fib) in the fall of 2010, about 15 years after my ASCT.
If you are a newly diagnosed myeloma patient and you are considering an ASCT, your age is probably in between 50-70. Probably the most serious multiple myeloma side effects is heart damage. According to research, you have about a 10% chance of arrhythmia post ASCT.
Did my ASCT cause my chronic A-fib?
Let’s look at the facts.
- My blood pressure has always been 120/80 or below-
- My cholesterol has always been normal-
- My BMI has always been under 25-
- I exercise regulary and have since college-
- I don’t smoke and I drink alcohol moderately-
- I underwent both adriamycin/doxorubicin and melphalan during my conventional cancer therapies in 1995-
- I underwent doxorubicin, cytoxan, busulfan and melphalan all within an 10 month period-
No lifestyle factors leading up to my chronic a-fib increased by risk and, according to the studies linked below both Anthracyclines and Melphalan chemotherapy regimens are known to causes arrhythmia aka A-fib.
I’m thinking that the evidence is leaning heavily toward chemotherapy causing my chronic A-fib.
But the thing that really gets me, the fact that really causes my anger this late stage multiple myeloma side effect didn’t have to happen. Just as important, stem cell transplants don’t increase your overall survival, your length of life according to research.
Don’t take my word for it, ask your oncologist.
To learn more about Stringent or Complete Response click now
Have you recently been diagnosed with myeloma? Are you considering an ASCT? Understand the risks and benefits, the pros and cons of possible MM therapies will help you make the right decisions for you. Scroll down the page, post a question or comment and I will reply to you ASAP.
Thank you,
David Emerson
- MM Survivor
- MMCancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- “Transplants are exhausting, and they are costly.” Is There A Better Way?
- Living With Chronic Atrial Fibrillation with Non-Conventional Therapy
- A Different kind of Second Opinion-Multiple Myeloma Cancer Coaching
Introducing a new entity: chemotherapy-induced arrhythmia
“Therefore, the purpose of this review was to collect and summarize the evidence of possible connections between different classes of chemotherapeutic agents and cardiac arrhythmias and A-fib.
Arrhythmias (A-fib) were reported as a side effect of many chemotherapeutic drugs. Anthracyclines are associated with atrial fibrillation (AF) at a rate of 2–10%…Melphalan is associated with AF in 7–12% of cases, but it does not appear to cause ventricular tachicardia...
Arrhythmias in the setting of hematopoietic cell transplants.
Prior studies report that 9-27% of persons receiving a hematopoietic cell transplant develop arrhythmias, but the effect on outcomes is largely unknown. We reviewed data from 1177 consecutive patients ⩾40 years old receiving a hematopoietic cell transplant at one center during 1999-2009. Transplant indication was predominately leukemia, lymphoma and multiple myeloma.
Overall, 104 patients were found to have clinically significant arrhythmia: 43 before and 61 after transplant. Post-transplant arrhythmias were most frequently atrial fibrillation (N=30), atrial flutter (N=7) and supraventricular tachycardia (N=11).
Subjects with an arrhythmia (A-fib) post transplant were more likely to have longer median hospital stays (32 days vs 23, P=<0.001), a greater probability of an intensive care unit admission (52% vs 7%; P<0.001), greater probability of in-hospital deaths (28% vs 3%, P<0.001), and greater probability of death within 1 year of transplant (41% vs 15%; P<0.001) compared with patients without arrhythmia at any time.
In a multivariate model including age at transplant, diagnosis, history of pretransplant arrhythmias, and transplant-related variables, post-transplant arrhythmias was associated with a greater risk for death within a year of transplant.
Our data suggest that arrhythmias after transplants are associated with significant morbidity and mortality. A prospective study of arrhythmia in the transplant setting is warranted.”
She suggested several potential reasons why a plant-based diet might be protective against Heart Failure. “Current theories include the effects of antioxidants and anti-inflammatory effects, which are highly abundant in plant-based diets,”
Heart Failure is one of the, if not they most common chronic disease in Americal today. Yet I read study after study (see below) that cite evidence-based, non-toxic therapies that reduce a heart failure patient’s risk of dying.
When I was diagnosed with chemotherapy-induced cardiomyopathy (heart disease), the first thing my cardiologist did was try to talk me into 1) metoprolol and 2) open heart surgery.
Are you kidding me? My BMI, BP, heart rate, etc. were all fine. While I did have an enlarged ascending aorta, Dr. Moudgil didn’t even attempt to talk about evidence-based, non-toxic therapies such as nutrition and sleep.
So I am taking on the task of researching and writing about evidence-based, non-toxic heart-healthy therapies. My goal is to manage my heart failure with non-toxic therapies such as diet, sleep, and nutritional supplemention.
According to the study linked below, a plant-based diet dramatically reduces your risk of heart failure compared to a “southern diet.”Because I already have heart faillure, my perspective is more about healing HF than preventing HF. Further, I’ll never change my diet to be plant-based 100% of the time. But I can increase my intake of fruits and veggies while I reduce my intake of animal fats and red meat.
I don’t mean to mix health with politics but personally, I think you’re free to live any way you want. If you want to live a heart un-healthy lifestyle by eating a poor diet, getting little sleep, drinking, smoking, etc. then I am fine with it. However, if you would like to learn how to rehab your heart disease then read on.
Update as of 2022- the past five annual echocardiograms indicate that all my heart metrics have either stabilized or improved. My ejection fraction, for example, has improved from 40 at diagnosis of CIC to 50-55 a few months ago.
No conventional medications- only heart healthy, nutrition, supplementation and lifestyle.
Are you a MM survivor/cancer survivor who underwent cardio-toxic chemotherapies? If you would like to learn more about evidence-based, non-toxic, non-invasive heart therapies, scroll down the page, post a question or comment and I will reply to you ASAP.
Recommended Reading:
Why sleeping less than 7 hours can lead to heart disease and Type 2 diabetes
“Decades of research has shown that chronic short sleep is associated with increased risk of clogged arteries, heart disease, and early mortality..”
Plant-Based Diet Linked to Lower Heart Failure Risk
“Plant-based diets are associated with a lower risk for incident heart failure (HF) in adults without known heart disease, new research suggests.
Researchers followed more than 16,000 adults (mean age, 64 years) with no known coronary heart disease (CHD) or HF at baseline, comparing those who adhered to a plant-based diet with those who consumed a Southern diet, consisting of more fried and processed foods and sweetened drinks.
They found that the plant-based diet was associated with a 41% lower risk for incident HF with the highest vs lowest adherence, while the Southern diet was associated with a 71% higher risk for HF with higher vs lower adherence, after adjustment for potential demographic, lifestyle, and medical confounders.
“The take-home message of our findings is to emphasize more vegetables, plant proteins like lentils, nuts, chickpeas, tofu, beans, etc, and limit consumption of meat; [this] is the future of health…”
Five Dietary Patterns
HF is projected to affect more than 8 million people by 2030, necessitating a “critical need” for population-based preventive strategies, the authors write.
Previous research has demonstrated inverse associations with incident hypertension in people adhering to the Mediterranean or DASH (Dietary Approaches to Stop Hypertension) diets; however, these studies were “limited to participants from populations that lacked racial and ethnic diversity,” the authors note…
“Our study focused on US American adults, both black and white, living in the stroke belt and continental US,” she added.
The researchers drew on data from the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study, a national cohort study consisting of 30,239 black and white adults (≥45 years) recruited from January 2003 to October 2007…
Participants were interviewed every 6 months. In those who reported hospitalization, medical records were retrieved and adjudicated based on signs/symptoms of HF, laboratory studies, and assessment of left ventricular function documented in the medical record.
Medical covariates included hypertension, dyslipidemia, diabetes, atrial fibrillation (AF), and chronic kidney disease (CKD).
Participants were followed for a median of 8.7 years, with telephone interviews conducted every 6 months.
Anti-inflammatory Effects
There were 363 new HF hospitalizations during the follow-up period.
In the fully adjusted analyses, there was a 41% lower risk for new HF hospitalizations for participants who were most adherent (Q4) to the plant-based dietary pattern, compared with those who were least adherent (Q1).
In contrast, highest adherence (Q4) to the Southern dietary pattern was associated with a 72% higher risk for HF hospitalization in models adjusted for age, sex, and race.
However, after adjustment for other potential confounders (education, income, region of residence, total energy intake, smoking, physical activity, and sodium intake), the association between the Southern diet and incident HF risk was attenuated and no longer statistically significant.
After multivariable adjustment, the researchers found no statistically significant associations among the remaining dietary patterns…
There was a 97% increased risk in adherents to the Southern dietary pattern for HFrEF, which was found to be statistically significant…
In contrast, a statistically significant interaction in the Southern dietary pattern was observed and showed a stronger positive association with HF in participants younger than 65 years…
“The Mediterranean diet is a much better option than the Southern dietary pattern, since it emphasizes healthy fats like olive oil, nuts, avocadoes, and fish, and recommends avoiding fried foods and red meat, which are central to the Southern diet,” she observed.
She suggested several potential reasons why a plant-based diet might be protective against HF. “Current theories include the effects of antioxidants and anti-inflammatory effects, which are highly abundant in plant-based diets,” she noted.
“Reactive oxygen species promote hypertrophy, aortic stiffness, interstitial fibrosis, and can potentially decrease myocardial contractility, all of which can contribute to the development of heart failure,” she explained.
“On the other hand, plant antioxidants decrease the amount of reactive oxygen species, and with plant-based diets, we can also see decreased serum concentrations of CRP [C-reactive protein], IL-6, [interleukin-6] and soluble intercellular adhesion molecule-1, which are inflammatory biomarkers,” she added.