“In a finding likely to add fuel to the debate over treatments for prostate cancer, proton-beam therapy provided no long-term benefit over traditional radiation despite far higher costs…”
You’ve been diagnosed with prostate cancer. Your oncologist explains his/her recommended therapy plan to you. You trust your oncologist so the plan must be right for you… right? If the therapy plan includes “proton-beam treatment,” maybe not. Ask your onc to show you studies or reports that clearly indicate that proton-beam therapy will manage your prostate cancer better than regular radiation. If your oncologist is honest with you, according to the article linked and excerpted below, he/she will not be able to. Keep in mind that proton-beam therapy will cost you and your insurance company much, much more than regular radiation.
Do you have a co-pay? Will you have to pay any of the treatment? Probably.
The newly diagnosed prostate cancer patient’s challenge is to learn of the many conventional (FDA approved) and evidence-based non-conventional therapies that may apply to their individual case.
I am a cancer survivor and cancer coach. If you would like help with evaluating your prostate cancer treatment plan, scroll down the page, post a question or comment and I will reply ASAP.
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
Proton-Beam Treatment for Prostate Tumors No Better Than Radiation, Study Says
“In a finding likely to add fuel to the debate over treatments for prostate cancer, proton-beam therapy provided no long-term benefit over traditional radiation despite far higher costs, according to a study of 30,000 Medicare beneficiaries published Thursday in the Journal of the National Cancer Institute.”
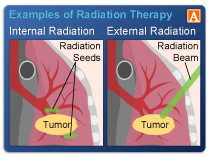
Proton radiotherapy uses atomic particles to treat cancer rather than X-rays and theoretically can target tumors more precisely. But it requires a particle accelerator roughly the size of a football field that typically costs about $180 million.
Faith in the superiority of proton therapy by some has sparked an arms race among major medical centers. Ten proton accelerators are in operation in the U.S., and nine more are in development, including two by the Mayo Clinic and one by Memorial Sloan-Kettering Cancer Center and a consortium of other hospitals in New York City.
Critics long have cited proton-beam therapy as a costly new technology with no proven advantage. Medicare pays over $32,000 per patient for proton therapy, compared with under $19,000 for radiation, according to the study.
Side effects of both can include incontinence and impotence, so researchers have sought potentially less-damaging therapies.
Proton-beam therapy has been the subject of heated debate among urologists, radiation oncologists and health-care cost analysts. The therapy isn’t considered more effective than standard radiation, or surgery, at stopping the cancer. And the patient experience is about the same as with standard radiation: Patients typically have daily treatments, Monday through Friday, for approximately eight weeks. Each treatment is painless, and lasts about five minutes.
The main debate has been over side effects.
There was no difference in the rate of other common side effects of radiation treatment for prostate cancer, including erectile dysfunction, hip fractures, gastrointestinal issues or musculoskeletal problems….”
“Background: Advances in radiation technology have transformed treatment options for patients with localized prostate cancer. The evolution of three-dimensional conformal radiation therapy and intensity-modulated radiation therapy (IMRT) have allowed physicians to spare surrounding normal organs and reduce adverse effects.
The introduction of proton beam technology and its physical advantage of depositing its energy in tissue at the end-of-range maximum may potentially spare critical organs such as the bladder and rectum in prostate cancer patients.
Data thus far are limited to large, observational studies that have not yet demonstrated a definite benefit of protons over conventional treatment with IMRT. The cost of proton beam treatment adds to the controversy within the field.
Methods: We performed an extensive literature review for all proton treatment-related prostate cancer studies. We discuss the history of proton beam technology, as well as its role in the treatment of prostate cancer, associated controversies, novel technology trends, a discussion of cost-effectiveness, and an overview of the ongoing modern large prospective studies that aim to resolve the debate between protons and photons for prostate cancer.
Results: Present data have demonstrated that proton beam therapy is safe and effective compared with the standard treatment options for prostate cancer. While dosimetric studies suggest lower whole-body radiation dose and a theoretically higher relative biological effectiveness in prostate cancer compared with photons, no studies have demonstrated a clear benefit with protons.
Conclusions: Evolving trends in proton treatment delivery and proton center business models are helping to reduce costs. Introduction of existing technology into proton delivery allows further control of organ motion and addressing organs-at-risk. Finally, the much-awaited contemporary studies comparing photon with proton-based treatments, with primary endpoints of patient-reported quality-of-life, will help us understand the differences between proton and photon-based treatments for prostate cancer in the modern era.”