Radiotherapy for prostate cancer was associated with higher risks of developing second malignancies of the bladder, colon, and rectum
If you undergo external beam radiotherapy for prostate cancer, according to the study below, you will increase your risk of a second primary cancer. The odds are pretty low but you have to add this increased risk to your thinking as you consider your diagnosis and therapy plan.
What side effects can occur from radiotherapy for prostate cancer?
Radiation therapy for prostate cancer can lead to both short-term and long-term side effects. Short-term side effects typically occur during the treatment period and may include:
- Fatigue: Feeling tired or exhausted is common during radiation therapy.
- Skin irritation: Irritation, redness, or blistering may occur in the pelvic area where the radiation is directed.
- Bowel changes: Diarrhea, urgency, or increased frequency of bowel movements can occur due to irritation of the rectum.
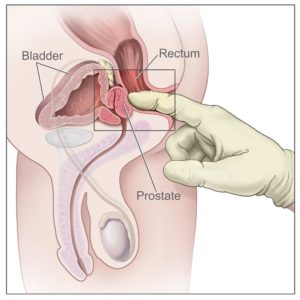
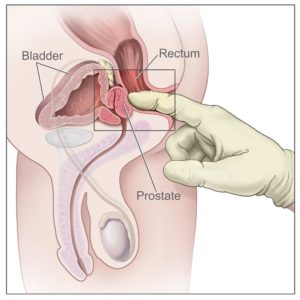
- Urinary symptoms: Increased frequency of urination, urgency, or discomfort during urination may occur.
Long-term side effects can develop months to years after treatment and may include:
- Erectile dysfunction: Radiation can affect blood flow to the penis, leading to difficulty achieving or maintaining an erection.
- Urinary problems: Radiation can cause urinary incontinence (leakage), urinary urgency, or difficulty urinating.
- Rectal problems: Long-term irritation or inflammation of the rectum can lead to bowel problems such as diarrhea, rectal bleeding, or narrowing of the rectum (stenosis).
- Secondary cancers: While rare, radiation therapy can increase the risk of developing secondary cancers in the pelvic area.
In my experience, conventional oncology understates collateral damage caused by toxic therapies. Radiation for PCa is a good example. If your oncologist mentions external beam radiotherapy to you he/she should mention those evidence-based therapies cited to reduce the risk of side effects caused by the radiation.
Resveratrol, HBOT, hydrogel, and other therapies can reduce or eliminate collateral damage caused by radiotherapy.
I am both a cancer survivor and cancer coach. I work with PCa patients to research and understand their therapy options and related strengths and weaknesses of those options.
Thank you,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
“Objective To determine the association between exposure to radiotherapy for the treatment of prostate cancer and subsequent second malignancies (second primary cancers)…
Results Of 3056 references retrieved, 21 studies were selected for analysis. Most included studies were large multi-institutional reports but had a moderate risk of bias. The most common type of radiotherapy was external beam; 13 studies used patients treated with surgery as controls and eight used patients who did not undergo radiotherapy as controls.
There was increased risk of
- cancers of the bladder,
- colorectum, and
- rectum,
after radiotherapy, compared with the risk in those unexposed to radiotherapy.
The odds of a second cancer varied depending on the type of radiotherapy: treatment with external beam radiotherapy was consistently associated with increased odds while brachytherapy was not. Among the patients who underwent radiotherapy, from individual studies, the highest absolute rates reported for bladder, colorectal, and rectal cancers were 3.8%, 4.2%, and 1.2%, respectively, while the lowest reported rates were 0.1%, 0.3%, and 0.3%…
Conclusion Radiotherapy for prostate cancer was associated with higher risks of developing second malignancies of the bladder, colon, and rectum compared with patients unexposed to radiotherapy, but the reported absolute rates were low. Further studies with longer follow-up are required to confirm these findings.
“Radiation-induced second malignancies (RISM) is one of the important late side effects of radiation therapy and has an impact on optimal treatment decision-making. Many factors contribute to the development of RISM such as age at radiation, dose and volume of irradiated area, type of irradiated organ and tissue, radiation technique and individual and family history of cancer.
Exact mechanism of RISM is unknown. But nowadays, it is a growing concern in oncology because of the increased number of cancer survivors and efforts are being made to prevent or decrease the incidence of RISM…
Conclusion
Radiotherapy has been considered as a double edged sword as it has a well-established role in the management of solid cancers but unfortunately it is likely to induce cancers years after the treatment. Risk of RISM is a main concern especially in pediatric population due to increase number of survivors. One of the main reasons is that patients who receive RT are at high risk of developing second cancer because of their lifestyle and genetic predisposition. This factor can be even more important than risk of radiation. But as of now, only little information is available about those factors which can modify the risk of second malignancies like genetic variants, lifestyle or environmental factors.
In many countries, recommendations on screening for second malignancies (especially breast cancer) have been developed for selected high-risk survivor groups. However, most guidelines are consensus-based rather than evidence-based. Effective screening is only possible with better understanding of the pathogenesis of treatment-related secondary cancers. Currently such knowledge is lacking, so there is a strong need for studies investigating the mechanisms by which different treatments affect the pathogenesis of second malignancies, the clinicopathological characteristics of treatment-related cancers and their prognosis. Integrated research involving clinical studies, radiobiology and physics are important to estimate and to reduce the risk of treatment related second cancers.”