Leave a Comment:
20 comments
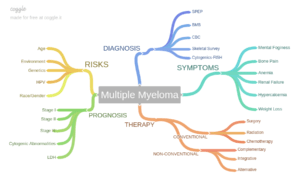
Hi David, we have communicated in the past. I was diagnosed with MM in Jan-Feb 2019 I have been in complete remission for about a year on maintenance revlimid, dietary changes, supplements. Trying to keep a healthy lifestyle. You mentioned to me a while ago about having a stem cell harvesting. My oncologist never brought it up I brought it up to him….referrals made.I have spoken to 2 MM specialists who recommend SCT. So I am going for the harvesting process next week. They are talking stem cell transplant sooner rather than later. Upon diagnosis I had a 14:16 translocation. However, my husband passed away in Nov 2020, I am considering downsizing and moving. I am just starting to get my life together a bit. I am still in complete remission on a revlimid wash for 3 weeks (have been on revlimid for a long time although for the last year on a reuced dose) for the harvesting and feeling very well. I feel I should wait to have the transplant. Huntsman Institute in Utah will store my stem cells for 5 yrs free of charge. I am thinking I can prolong my remission naturally and stay on an even smaller dose of Revlimid or possibly Pomalyist. Next week I do preliminary testing and start injections of Neupogen…they are taking into consideration a longer time may be possible to collect enough cells because of being on the Revlimid for 2 yrs. Interestingly my local oncologist once told me he compared MM to a chronic disease like diabetes….meaning when one med stops working there are many other medications to try. I was a bit surprised he did not recommend the SCT sooner and I approached him after you encouraged the harvesting.
ReplyHi Linda-
I will reply to your post directly via your email address. thanks.
David Emerson
Reply[…] ASCT Now or Later? Makes No Difference in Multiple Myeloma […]
Reply[…] ASCT Now or Later? Makes No Difference in Multiple Myeloma […]
Reply[…] ASCT Now or Later? Makes No Difference in Multiple Myeloma […]
Reply[…] ASCT Now or Later? Makes No Difference in Multiple Myeloma […]
Reply[…] ASCT Now or Later? Makes No Difference in Multiple Myeloma […]
Reply[…] ASCT Now or Later? Makes No Difference in Multiple Myeloma […]
Reply[…] ASCT Now or Later? Makes No Difference in Multiple Myeloma […]
Reply[…] ASCT Now or Later? Makes No Difference in Multiple Myeloma […]
Reply[…] ASCT Now or Later? Makes No Difference in Multiple Myeloma […]
ReplyIve been in Remission for 20 years. 2/24/22018 Have a lot of.
Other Health problems. But the MM IS STILL IN Remission. I thank God every day
Hi Rickie-
Congrats on your long-term MM remission. With your permission, I would like to write a blog post about your experience. Can you tell me more about your diagnosis, type, stage, side effects, therapies, etc.?
Thank you,
David Emerson
ReplyHi! I am so pleased I found this. I was diagnosed in Oct 2016 with Myeloma in my spine. I have been on chemo since November and I am reluctant to have sct. I have an appointment on Monday at St Barts to talk to the team about the sct. My whole being is telling me not to have it. I’m looking for all the advice that I can find, for and against…..my train of thought is, if my myeloma is low and I am doing ok, why do I need to put myself through months of hell, to get a remission that isn’t guaranteed . The side effects, to me, outweigh the remission. I have kidney problems anyway and I’m sure I wouldn’t be able to cope with sct.
St
Hi Trudie-
I am sorry to learn of your MM diagnosis. Let me go over a few concepts that should help you with your appt. this Monday. In general, there is a long and growing list of FDA approved therapies to manage MM and there is a long and growing list of evidence-based but non-conventional therapies that fight MM. Your job is to use the best of either/or depending on your situation.
For instance-
“with Myeloma in my spine…” Depending on the bone damage in your spine caused by your MM, you may benefit from local radiation. You may want to learn about Kyphoplasty, again for your spine.
If you can stabilize your MM in your spine and if your induction chemotherapy that you have been taking since November helps you reach remission then you don’t need to consider more therapy. Your oncology team might encourage an ASCT because a) this procedure is the standard of care and b) studies say it gives the longest “progression-free survival.” Not longest length of life but the longest remissions.
You are correct in your thinking that an ASCT is aggressive chemotherapy and therefore lots of toxicity. Toxicity causes short, long-term and late stage side effects. You are correct that increased toxicity and an ASCT can lead to “months of hell.”
You mentioned that your MM is low. Do you know what stage you were at when you were diagnosed? How old are you and how is your health otherwise? I don’t mean to be nosey. The more info I know the more info I can offer.
You signed up for the webinar. You will learn about the MM Cancer Coaching program. Let me know if you have any questions.
Thanks.
David Emerson
ReplyHi David,
Can you please resend as I did not receive it yet.
Thanks
I am a mm patient for the last two years. I stopped taking chemo medicines for the last one and a half years and has started working on alternative options and diet. It would be great of you, if you could advice me how to go further and work on it without any chemo.
Well when I was diagnosed my Mspike was 6.2 and after one year of treatment it was 1.25 and now after no treatment it is 1.87.
The Ig g was 6570 and after treatment it was 1650 and now it is 2300.
My Hb is 14.1, WBC and platelets are below normal. I don’t have any pain and I am living a normal lifestyle but worried about the proteins numbers and concerned.
I want to explore alternative options. You have been a role model to others and gives me a hope knowing your survival period and strong thoughts gives me encouragement.
Great regards
Sehgal
Hi Sehgal-
I replied to your first contact by sending you the link to my webinar. I hope you can watch the webinar and get the MM CC program.
Regarding your m-spike and IgG numbers, as you probably know you are doing well to have lowered your numbers yet you may be coming out of remission. Watch the webinar and let me know what you think.
thanks
David
ReplyI am a mm patient for the last two years. I stopped taking chemo medicines for the last one and a half years and has started working on alternative options and diet. It would be great of you, if you could advice me how to go further and work on it without any chemo.
Great regards
Sehgal
Hi Sehgal-
I am sorry to learn of your MM diagnosis. Did you stop taking chemo because you reached remission? Are you experiencing any side effects such as nerve pain?
I have remained in complete remission since ’99 by following a sort of evidence-based, anti-MM program of nutrition, supplementation, bone health, etc. I have created an 11 step program for other MMers to follow. To watch the free webinar about the program click the link below.
https://peoplebeatingcancer.org/free-multiple-myeloma-webinar/
Let me know if you have any questions.
David Emerson
Reply