Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Autologous Stem Cell Transplant for Multiple Myeloma Explained
Autologous Stem Cell Transplant for Multiple Myeloma Explained
Abnormalities in multiple myeloma patients with (4;14) and (14;16) and loss of 17p13 confirmed poor prognosis with (stem cell transplant) high dose therapy.
Autologous Stem Cell Transplantation (ASCT) for the multiple myeloma patient is high-risk, high-reward therapy. The single most important thing for newly diagnosed MMers to get is a thorough diagnosis. Not just blood work. As you can see from the facts below, newly diagnosed MMers must diagnose their molecular subtyping. The challenge to the newly diagnosed MMer is that he/she doesn’t know what to ask or what to learn in order to decide in favor of, or against ASCT.
To quote the list below “Disease biology is reflected on the molecular subtype of myeloma and the presence or absence of secondary cytogenetic abnormalities.” Your survival statistics all depend on your molecular subtype.
I am both a long-term MM survivor and MM Cancer Coach. I have lived in complete remission from my MM since ’99 by living an evidence-based yet non-conventional, anti-MM lifestyle of nutrition, supplementation, lifestyle and more. Please watch the free webinar linked on the right of this page. Let me know if you have any questions.
Thank you,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Multiple Myeloma- Vitamin D Deficiency
- Pre-Autologous Stem Cell Transplant Chemotherapy- More is Not better.
- Multiple Myeloma-Newly Diagnosed, Post SCT and Relapsed?
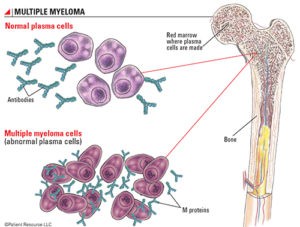
Multiple myeloma
“Dr. Stephen Cohen–Have you ever wanted to read the notes and observations of a practicing compassionate and empathetic doctor who has cared for cancer patients for over 40 years? Well, now you can! Dr. Stephen Cohen, a medical oncologist and hematologist practicing in San Antonio, Texas, has kept a daily journal of interesting medical info and tidbits he encounters day to day from his personal experiences with patient care, professional journals he reads, and medically relevant information on all subjects that he comes across.”
Survival varies depending upon a host of factors: the stage of disease, biology including cytogenetic abnormalities and response to therapy.
In patients under 60 years of age median 10-year survival approximately 30% (Kumar SK et al).
Overall survival is greater than 8 years currently (2013)
Disease biology is reflected on the molecular subtype of myeloma and the presence or absence of secondary cytogenetic abnormalities.
A five-year survival rate of greater than 70% is present in transplant-eligible patients, 50% in elderly transplant ineligible patients.
Unfortunately, approximately 25% of patients have a median survival of 2 years or less.
Plasma cells secrete monoclonal immunoglobulin, IgG in about 60%, IgA in about 20%, for light chains in 20%, IgD in 2%, and OgM in 0.5%, and in about 2-3% no detectable M protein.
Abnormalities in (4;14) and (14;16), and loss of 17p13 confirmed poor prognosis with (stem cell transplant) high dose therapy.
Deletion 17p suggests a low likelihood of long-term disease control with traditional approaches of induction, consolidation, and maintenance.
Overall survival for patients with 17p deletion have half the survival than patients who do not have that.
Poor prognosis associated with decreased serum albumin, increased beta 2 microglobulin, the presence of abnormal cytogenetics, increased interleukin 6, increased C reactive protein, high lactate dehydrogenase, extramedullary disease, insufficiency, high serum free light chains, abnormal kappa/lambda ratio, increased plasma cell labeling index, cytogenetic changes and the presence of circulating plasma cells.
Cytogenetic abnormalities on conventional studies indicate the presence of a high proliferative rate malignancy with poor prognosis.
Probable change of infections related to progressively aggressive treatments.
Invasive aspergillosis after hematopoietic stem cell transplant (HSCT) increasingly common and the risk is 4.5 times higher than patients with chronic myelogenous leukemia in chronic phase (Marr KA).
Allogeneic BMT achieves long-term disease-free survival of 15%-20% of patients.
Two transplantations with high dose melphalan associated with a seven-year event-free and overall survival rates of 20 and 40%, respectively.
The event-free and overall survival rates for two high-dose transplantations are double over single transplantations.
The use of thalidomide in intensive melphalan chemotherapy with stem cell transplantation increases the rate of complete remission and event-free survival in previously untreated patients but does not increase overall survival.
Stem cell transplant most common indication.
Response rates are not valid surrogates for determining survival in myeloma studies.
Complete response rate requires the absence of original monoclonal protein in serum and urine that is maintained for a minimum of six weeks, less than 5% plasma cells in the bone marrow, no increase in size and number of lytic lesions, and disappearance of the soft tissue plasmacytomas.
Partial response requires 50% or greater reduction in the level of the serum monoclonal protein, maintain for a minimum of six weeks, reduction in 24 hour urinary light chain excretion by 90% or greater to 200 mg, maintain for a minimum of six weeks, for patients with non-secretory disease. 50% or greater reduction in plasma cells in the bone marrow, maintain for a minimum of six weeks, a 50% or greater reduction in the size of soft tissue plasmacytomas, and no increase in the size of a number of lytic bone lesions.
Candidates for auto-transplantation should not receive induction therapy with stem cell damaging agents, such as melphalan, which can preclude stem cell harvest.
Use of high dose therapy and autologous bone marrow transplant as part of induction therapy associated with an improved response, but not a survival advantage for early vs late transplantation.
The administration of high dose melphalan for transplant patients is 200 mg per meter squared as the standard dose.
ASCT after high dose chemotherapy associated with a median survival of more than 5 years.
ASCT associated with a 3-5% mortality.
Autologous stem cell transplantation (ASCT) can be performed either early in the disease or at the time of first relapse with both strategies being useful.
A short course of induction therapy, 3-6 months, followed by autologous stem cell transplantation (ASCT) without maintenance therapy results in very good partial responses of 50-60% and complete response rates of 25-50% and a median time to progressive disease around 2 years.
Tandem ASCT or maintenance following ASCT improves progression free survival and overall survival, but the benefits appear to be primarily among those patients obtaining less than a (VGPR) very good partial response.
Patients treated with autologous stem cell transplant and with progressive disease are at increased risk of early death from infection.
The 4-year overall survival (OS) rate is 82.3% among patients diagnosed with multiple myeloma at age 65 years or younger, who are eligible for autologous stem cell transplantation (ASCT), according to a retrospective study.