Progression to adenocarcinoma (Barrett’s esophagus to esophageal cancer) is not universal, suggesting that an intensive surveillance program may be sufficient for some patients…
If you’ve been diagnosed with Barrett’s esophagus, with high-grade dysplasia you have several challenges to consider. First and foremost you may be concerned that your BE may develop into esophageal cancer. Secondly, according to the first article linked below, esophagectomy, surgical removal of the BE, can have serious complications. PDT and RFA may be options for your considerations.
I am a cancer survivor and cancer coach. My role is to research evidence-based therapies for people in your situation in order to help you think through the best options for your goals. My perspective is that of a cancer survivor, not an oncologist. I consider both conventional (FDA approved) and evidence-based non-conventional therapies.
What are possible therapies for Barrett’s Esophagus?
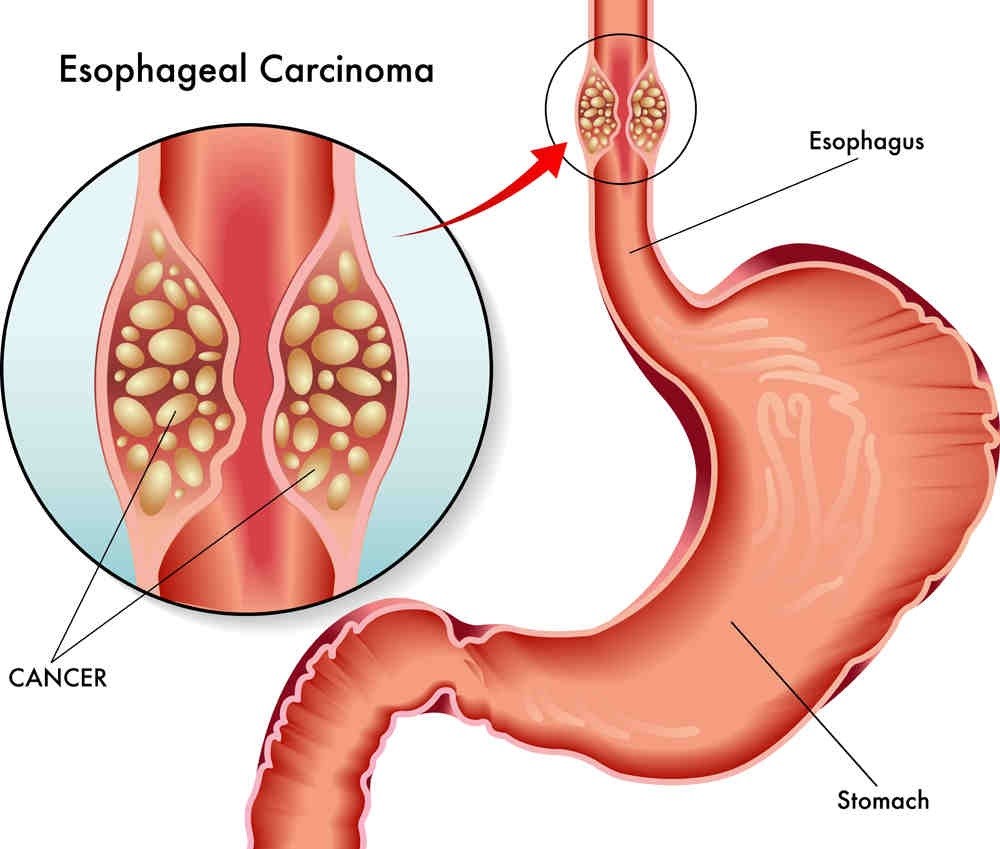
Barrett’s esophagus is a condition in which the lining of the esophagus changes, becoming more like the lining of the small intestine. It is often associated with chronic gastroesophageal reflux disease (GERD). While there is no cure for Barrett’s esophagus, various therapies and management strategies aim to prevent complications and monitor the condition. Here are some common approaches:
- Medications:
- Proton Pump Inhibitors (PPIs): These drugs reduce the production of stomach acid and are often prescribed to manage GERD symptoms and prevent further damage to the esophagus lining.
- H2 blockers: Another class of medications that can reduce stomach acid production.
- Lifestyle and Dietary Changes:
- Diet modification: Avoiding acidic and spicy foods, chocolate, caffeine, and fatty meals may help reduce symptoms.
- Weight management: Losing excess weight can decrease abdominal pressure and reduce reflux.
- Elevating the head of the bed: This can help prevent stomach acid from flowing back into the esophagus during sleep.
- Endoscopic Surveillance:
- Regular endoscopic examinations are typically recommended to monitor the condition and detect any signs of dysplasia or cancer early.
- Endoscopic procedures may also include treatments such as ablation or mucosal resection for precancerous lesions.
- Radiofrequency Ablation (RFA):
- RFA is an endoscopic procedure that uses radiofrequency energy to remove abnormal cells in the esophagus lining. It is often used for treating Barrett’s esophagus with dysplasia.
- Photodynamic Therapy (PDT):
- PDT involves the use of a photosensitizing agent and a laser to destroy abnormal cells. This therapy is less commonly used compared to other methods.
- Surgery:
- In some cases, surgical intervention may be considered, especially if there is a high-grade dysplasia or cancer. Surgical options may include fundoplication or esophagectomy.
It’s crucial to note that the choice of therapy depends on various factors, including the severity of Barrett’s esophagus, the presence of dysplasia, and individual patient characteristics.
If you have been diagnosed with GERD, BE or EC, please scroll down the page, post a question or comment and I will reply to you ASAP.
Thank you,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
To Learn More about Barrett’s Esophagus, read the posts below-
“The management of patients with Barrett’s esophagus with high-grade dysplasia is controversial. Those who are good operative candidates have traditionally been offered surgical resection because of the high risk that adenocarcinoma is already present or will soon develop [1-4]. On the other hand, progression to adenocarcinoma is not universal, suggesting that an intensive surveillance program may be sufficient for some patients. Furthermore, esophagectomy is associated with significant short- and long-term morbidity and a 3 to 13 percent rate of surgical mortality depending in part upon the surgical expertise and hospital volume…
An alternative approach is based upon the observation that the destruction of intestinal metaplasia using a variety of chemical and thermal methods may be accompanied by regrowth of normal-appearing squamous epithelium, particularly if the patients are treated with proton pump inhibitors to keep them achlorhydric. Of the many endoscopic techniques that are capable of ablating columnar mucosa containing high-grade dysplasia, photodynamic therapy has attracted attention due to its novel approach and early success [5-10]…”
“Photodynamic therapy (PDT) is a drug and device therapy using photosensitizer drugs activated by laser light for mucosal ablation. Porfimer sodium PDT has been used extensively with proven long-term efficacy and durability for the ablation of Barrett esophagus and high-grade dysplasia. and early esophageal adenocarcinoma.
However, continued use is hampered by an associated stricture risk and prolonged photosensitivity (4-6 weeks). Promising single-center European studies using other forms of PDT, such as aminolevulinic acid PDT, have not been replicated elsewhere, limiting the widespread use of other forms of PDT. Future use of PDT in esophageal disease depends on the development of improved dosimetry and patient selection to optimize treatment outcomes while minimizing adverse events and complications.”
“Turmeric obtained from the rhizomes of Curcuma longa has been used in the prevention and treatment of many diseases since the ancient times. Curcumin is the principal polyphenol isolated from turmeric, which exhibits anti-inflammatory, antioxidant, antiapoptotic, antitumor, and antimetastatic activities.
The existing evidence indicates that curcumin can exert a wide range of beneficial pleiotropic properties in the gastrointestinal tract, such as protection against reflux esophagitis, Barrett’s esophagus, and gastric mucosal damage induced by nonsteroidal anti-inflammatory drugs (NSAIDs) and necrotizing agents.
The role of curcumin as an adjuvant in the treatment of a Helicobacter pylori infection in experimental animals and humans has recently been proposed. The evidence that this turmeric derivative inhibits the invasion and proliferation of gastric cancer cells is encouraging and warrants further experimental and clinical studies with newer formulations to support the inclusion of curcumin in cancer therapy regimens.
This review was designed to analyze the existing data from in vitro and in vivo animal and human studies in order to highlight the mechanisms of therapeutic efficacy of curcumin in the protection and ulcer healing of the upper gastrointestinal tract, with a major focus on addressing the protection of the esophagus and stomach by this emerging compound…”