- You are here:
- Home »
- Blog »
- Uncategorized »
- Bladder Cancer- Observation?
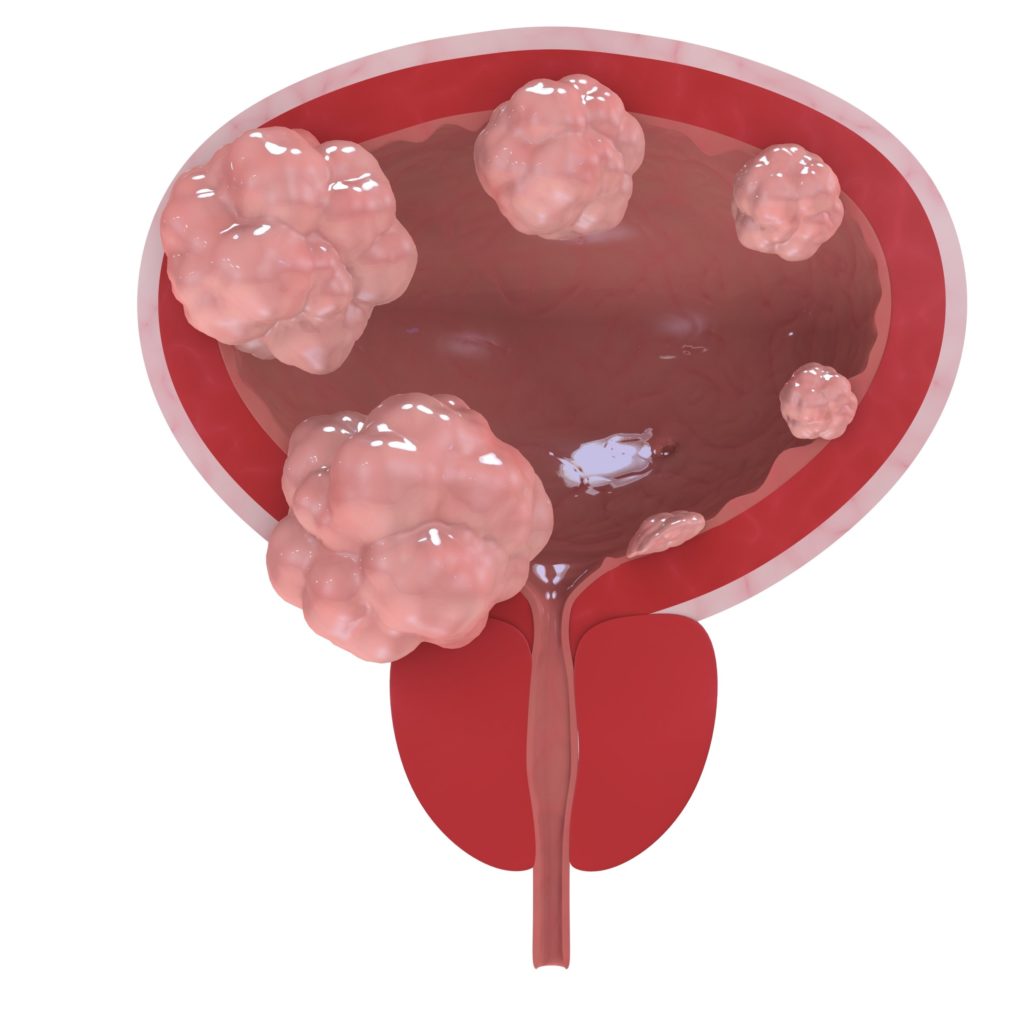
Bladder Cancer- Observation?
“Bladder cancer has the highest lifetime treatment cost of all cancers, with substantial economic burden throughout the entire disease course…with the focus on limiting overuse of surveillance testing and treatment, may mitigate associated increasing costs of care.”
The two articles linked and excerpted below offer up two opposing point illustrating the conventional and non-conventional sides of bladder control when discussing bladder cancer.
The first article about bladder cancer talks about how expensive observation is after an early stage bladder cancer diagnosis. The article assumes all conventional, FDA approved therapies. To be sure, conventional therapies, conventional diagnostic testing, conventional everything is expensive.
But what about evidence-based non-conventional therapies shown to reduce the risk of bladder cancer?
By evidence-based I mean those therapies supported by research. By non-conventional, I mean those therapies that have not been approved by the Food and Drug Administration (FDA).
To be clear, I am not an oncologist. I am a long-term survivor of a very different cancer called multiple myeloma. I’m simply saying that I have learned to think outside the conventional “standard-of-care” therapy box.
Scroll down the page, post a question or comment and I will reply to you ASAP.
Thank you,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Cancer Coaching-Ballooning Survivor population in the U.S
- Bladder Cancer – Conventional with Non-Conventional
- Bladder Cancer- “No Sex Drive/no Desire for Sex at All…”
Overuse’ of Surveillance Testing Observed in Low-Grade Non-Muscle Invasive Bladder Cancer
“A large study showed an increase in surveillance testing over time among patients with low-grade papillary stage Ta non-muscle invasive bladder cancer (NMIBC).
The study also revealed a 60% increase in the cost of care during the first year after diagnosis. These findings were published in JAMA Network Open.
“Bladder cancer has the highest lifetime treatment cost of all cancers, with substantial economic burden throughout the entire disease course,” the researchers wrote. “Efforts to improve adherence to current practice guidelines, with the focus on limiting overuse of surveillance testing and treatment, may mitigate associated increasing costs of care.”
For this study, the researchers examined surveillance and treatment patterns in patients who were diagnosed with low-grade Ta tumors and included in the SEER-linked Medicare database from 2004 to 2013. The researchers also reviewed Medicare claims data through 2014…
Rates of cystoscopy increased over time, from 79.3% in 2004 to 81.5% in 2013 (P =.007). Patients received a median of 3 cystoscopies per year after diagnosis.
Use of CT or MRI for upper tract imaging also increased, from 30.4% in 2004 to 47.0% in 2013 (P <.001). Patients received a median of 2 scans per year.
The use of urine-based testing increased as well, from 44.8% in 2004 to 54.9% in 2013 (P <.001). Patients had a median of 2 to 3 urine-based tests per year…
As for treatment, 17.2% of patients received intravesical bacillus Calmette-Guérin, 6.1% received intravesical chemotherapy, and 89.7% underwent at least 1 subsequent transurethral resection of the bladder tumor.
Overall, 1.7% of patients experienced disease recurrence, and 0.4% experienced progression.
The total median cost of care at 1 year after diagnosis increased by 60% over the study period, from $34,792 in 2004 to $53,986 in 2013…
Disclosures: Some study authors declared affiliations with biotech, pharmaceutical, and/or device companies. Please see the original reference for a full list of disclosures.
Reference
Bree KK, Shan Y, Hensley PJ, et al. Management, surveillance patterns, and costs associated with low-grade papillary stage Ta non-muscle-invasive bladder cancer among older adults, 2004-2013. JAMA Netw Open. Published online March 18, 2022. doi:10.1001/jamanetworkopen.2022.3050
Curcumin inhibits bladder cancer progression via regulation of β-catenin expression
“Bladder cancer has a considerable morbidity and mortality impact with particularly poor prognosis. Curcumin has been recently noticed as a polyphenolic compound separated from turmeric to regulate tumor progression. However, the precise molecular mechanism by which curcumin inhibits the invasion and metastasis of bladder cancer cells is not fully elucidated.
In this study, we investigate the effect of curcumin on the bladder cancer as well as possible mechanisms of curcumin…
In addition, bladder cancer cell lines T24 and 5637 cells were treated with different concentrations of curcumin. The cytotoxic effect of curcumin on cell proliferation of T24 and 5637 cells was measured by 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide assay.
Furthermore, curcumin inhibited the cell proliferation of T24 and 5637 cells, and curcumin reduced the migration and invasive ability of T24 and 5637 cells via regulating β-catenin expression and reversing epithelial–mesenchymal transition. Curcumin may be a new drug for bladder cancer.”
Chemopreventive effect of omega-3 polyunsaturated fatty acids and atorvastatin in rats with bladder cancer
“Bladder cancer remains a huge concern for the medical community because of its incidence and prevalence rates, as well as high percentage of recurrence and progression. Omega-3 polyunsaturated fatty acids and atorvastatin proved anti-inflammatory effects through peroxisome proliferator-activated receptor gamma mechanism…
In this study, bladder cancer was induced in rats by the chemical carcinogen N-butyl-N-(4-hydroxybutyl)nitrosamine. Omega-3 polyunsaturated fatty acids (docosahexaenoic acid and eicosapentaenoic acid: 2:3 w/w; 1200 mg/kg) and/or atorvastatin (6 mg/kg) were given orally daily to rats for eight consecutive weeks concomitantly with N-butyl-N-(4-hydroxybutyl)nitrosamine and continued for further 4 weeks after cessation of N-butyl-N-(4-hydroxybutyl)nitrosamine administration.
The study of the molecular mechanisms illustrated downregulation of COX-2 and P53 (mutant) genes and suppression of transforming growth factor beta-1 and the lipid peroxidation product malondialdehyde in serum of rats of the three treated groups.
This chemopreventive effect was confirmed by and associated with lower level of bladder tumor antigen in urine.
However, the combined treatment with both drugs exhibited the major protective effect and nearly corrected the dyslipidemia that has been induced by N-butyl-N-(4-hydroxybutyl)nitrosamine.
Collectively, omega-3 polyunsaturated fatty acids and atorvastatin, besides having anti-inflammatory properties, proved a chemopreventive effect against bladder cancer, which nominates them to be used as adjuvant therapy with other chemotherapeutics.
Sulforaphane suppresses the viability and metastasis, and promotes the apoptosis of bladder cancer cells by inhibiting the expression of FAT‑1
“FAT atypical cadherin 1 (FAT1) regulates complex mechanisms for the promotion of oncogenesis or the suppression of malignancies. Sulforaphane (SFN) has antioxidant and anti‑tumor activities.
The present study investigated the roles of SFN and FAT1 in bladder cancer (BC). The expression of FAT1 in BC cell lines and tissues was measured by western blot analysis and reverse transcription‑quantitative PCR (RT‑qPCR).
The association between FAT1 expression and the 5‑year survival rate of patients with BC was evaluated. The viability of and FAT1 expression in T24 and SW780 cells exposed to various concentrations of SFN were detected by MTT assay, and western blot analysis and RT‑qPCR, respectively…
The results revealed that FAT1 expression in BC cells and tissues was increased, and patients with a high FAT‑1 expression had a shorter 5‑year survival time than those with a low FAT‑1 expression. BC cell viability and FAT1 expression were suppressed by SFN in a concentration‑dependent manner.
The knockdown of FAT1 inhibited the viability, migration and invasion, and promoted the apoptosis of BC cells, whereas the overexpression of FAT1 produced opposite effects.
In addition, cells exposed to SFN exhibited a reduced viability, migration, invasion and an increased apoptosis, effects which were promoted by FAT1 knockdown; however, the overexpression of FAT1 blocked the above‑mentioned effects of SFN on the cells.
On the whole, the present study demonstrates that SFN suppresses the progression of BC by inhibiting the expression of FAT‑1; thus, SFN may be used as a potential drug for the treatment of BC.”

