
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Axillary Dissection vs No Axillary Dissection-Invasive Breast Cancer and Sentinel Node Metastasis
Axillary Dissection vs No Axillary Dissection-Invasive Breast Cancer and Sentinel Node Metastasis
Sentinel lymph node dissection (SLND) accurately identifies nodal metastasis of early breast cancer, but it is not clear whether further nodal dissection affects survival.
New research titled “Axillary Dissection vs No Axillary Dissection in Women With Invasive Breast Cancer and Sentinel Node Metastasis” concludes that in a certain group of women with invasive breast cancer a full axillary lymph node dissection is not necessary when one or two infected sentinel lymph nodes are found.
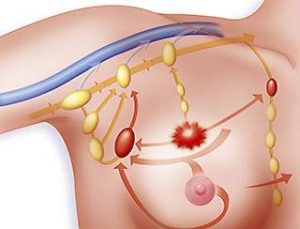 If widely accepted this is a huge departure from years of belief that if any cancer is found in the sentinel node or nodes that a full axillary lymph node dissection must be performed to improve survival chances. This is good news for this group of women because the risk of lymphedema is greatly reduced. Lymphedema can be a major problem with effects that last for years.
If widely accepted this is a huge departure from years of belief that if any cancer is found in the sentinel node or nodes that a full axillary lymph node dissection must be performed to improve survival chances. This is good news for this group of women because the risk of lymphedema is greatly reduced. Lymphedema can be a major problem with effects that last for years.
The women included in the study had what was believed to be stage 1 or 2 breast cancer and underwent a sentinel node biopsy that revealed either one or two cancerous sentinel nodes. They also had to have had a lumpectomy (not a mastectomy) and undergo whole breast radiation. They were not included in the study if they had any palpable lymph nodes before the surgery or if they had chemotherapy before surgery.
One of the most stressful cancer moments for me was when I awoke from surgery not knowing if there had been cancer in my lymph nodes. At that time (2003) and until the current time, if I had been found to have even one cancerous sentinel node, I would have awakened from my surgery minus all of my underarm lymph nodes. Today, if I had a surgeon who subscribes to the validity of this research, I could potentially keep those nodes and have an equally good chance of survival without the much higher likelihood of lymphedema.
An important thing to take into consideration is that most of these women also had adjuvant chemotherapy and/or hormonal therapy after their surgery, although I was surprised in reading the full text that it did not seem to be required to be part of the study.
Mary Miller- Breast Cancer Profile in Courage
Axillary Dissection vs No Axillary Dissection in Women With Invasive Breast Cancer and Sentinel Node MetastasisA Randomized Clinical Trial
“Context Sentinel lymph node dissection (SLND) accurately identifies nodal metastasis of early breast cancer, but it is not clear whether further nodal dissection affects survival.
Objective To determine the effects of complete axillary lymph node dissection (ALND) on survival of patients with sentinel lymph node (SLN) metastasis of breast cancer…
Interventions All patients underwent lumpectomy and tangential whole-breast irradiation. Those with SLN metastases identified by SLND were randomized to undergo ALND or no further axillary treatment. Those randomized to ALND underwent dissection of 10 or more nodes. Systemic therapy was at the discretion of the treating physician.
Main Outcome Measures Overall survival was the primary endpoint, with a noninferiority margin of a 1-sided hazard ratio of less than 1.3 indicating that SLND alone is non-inferior to ALND. Disease-free survival was a secondary endpoint.
Results Clinical and tumor characteristics were similar between 445 patients randomized to ALND and 446 randomized to SLND alone. However, the median number of nodes removed was 17 with ALND and 2 with SLND alone. At a median follow-up of 6.3 years (last follow-up, March 4, 2010), 5-year overall survival was 91.8% (95% confidence interval [CI], 89.1%-94.5%) with ALND and 92.5% (95% CI, 90.0%-95.1%) with SLND alone; 5-year disease-free survival was 82.2% (95% CI, 78.3%-86.3%) with ALND and 83.9% (95% CI, 80.2%-87.9%) with SLND alone. The hazard ratio for treatment-related overall survival was 0.79 (90% CI, 0.56-1.11) without adjustment and 0.87 (90% CI, 0.62-1.23) after adjusting for age and adjuvant therapy.
Conclusion Among patients with limited SLN metastatic breast cancer treated with breast conservation and systemic therapy, the use of SLND alone compared with ALND did not result in inferior survival.
Routinely Removing Axillary Lymph Nodes May Not Make Sense for Many Women
“A study, called the Z0011 trial, suggests that routinely removing the axillary lymph nodes during surgery to remove early-stage breast cancer may not make sense for many women. The axillary lymph nodes are the lymph nodes under the arm. Surgically removing these lymph nodes is called axillary lymph node dissection (ALND).
When early-stage breast cancer is removed, the lymph node or nodes closest to the cancer — the sentinel node(s) — often is removed and sent to a pathologist for evaluation. Removing just these nodes is called sentinel lymph node biopsy or sentinel lymph node dissection (SLND).
If cancer cells are in the sentinel node, it means the cancer has spread beyond the breast. So more treatment may be needed to reduce the risk of the cancer coming back (recurrence). If cancer is in the sentinel node, there are several treatment choices to reduce recurrence risk:
- axillary lymph node dissection
- axillary radiation therapy (radiation therapy to underarm lymph nodes)
- chemotherapy
- targeted therapy
- hormonal therapy (if the cancer is hormone-receptor-positive)
Lymphedema is one risk of axillary lymph node dissection. Lymphedema is swelling of the arm, hand, chest wall, and/or back caused by lymph fluid collects in tissue after lymph nodes are removed. Edema is the medical term for swelling, so swelling caused by lymph fluid is “lymphedema.” Experts estimate that from 5% to 40% of women will experience some level of lymphedema after breast cancer surgery. Having sentinel lymph node dissection instead of axillary lymph node dissection can lower the risk of lymphedema, but there is still some risk. Research shows that between 4% and 13% of women will experience lymphedema after sentinel lymph node dissection. Besides lymphedema, problems moving the arm and shoulder can be other axillary lymph node dissection side effects.
Because of these possible side effects, axillary lymph node dissection makes sense only for women who will clearly benefit from the surgery. This study wanted to know if women who had axillary lymph node dissection had better outcomes than women who had only sentinel lymph node dissection.
This study looked at 891 women diagnosed with early-stage breast cancer. None of the women’s lymph nodes felt abnormal in any way (they had no palpable adenopathy) and the cancer wasn’t considered aggressive.
All the women had:
- lumpectomy to remove the cancer
- sentinel lymph node dissection that found cancer in the sentinel node
- whole-breast radiation therapy after surgery
Many but not all of the women also received chemotherapy and/or hormonal therapy after surgery.
After radiation therapy, the women were split into two groups. One group had axillary lymph node dissection and the other group had no more surgery.
After about 6 years, the researchers found no differences in outcomes between the two groups.
- 92.5% of women who had only sentinel lymph node dissection were alive after 5 years (called overall survival) compared to 91.8% of women who had axillary lymph node dissection
- 83.9% of women who had only sentinel lymph node dissection were alive with no cancer recurrence after 5 years (called progression-free survival) compared to 82.2% of women who had axillary lymph node dissection
An earlier analysis of the results also found:
- 2.1% of women who had only sentinel lymph node dissection had a cancer recurrence within 5 years compared to 3.7% of women who had axillary lymph node dissection
- 1.3% of women who had only sentinel lymph node dissection had cancer come back in the lymph nodes compared to 0.6% of women who had axillary node dissection
The researchers planned to enroll 1,900 women in the study. Still, when the analysis showed that women who had axillary node dissection didn’t do any better than women who only had sentinel node dissection, the study was stopped early.
In the past, most doctors thought that axillary lymph node dissection made sense for many women diagnosed with early-stage breast cancer that had spread to nearby lymph nodes. But now many doctors think that treatments such as chemotherapy and hormonal therapy after surgery may make axillary lymph node dissection unnecessary for some women. The results of this study suggest that this is true. Still, it’s important to remember that the researchers followed the women in the study for only about 6 years. Longer follow-up time would boost confidence in the conclusions drawn from the study.
It’s also important to know that the results of this study apply only to women with the same characteristics as the women in this study:
- lymph nodes seemed normal before surgery
- had a lumpectomy, chemotherapy, and radiation
These study results do NOT apply to:
- women with lymph nodes that are enlarged or suspicious based on a doctor’s exam or testing before surgery
- women who had a mastectomy with or without chemotherapy and radiation
If you’ve been diagnosed with early-stage breast cancer, sentinel node biopsy may be done as part of your surgery. If cancer cells are found in the sentinel node, your doctor will consider all the details of your situation, including your age and the characteristics of the cancer (size, stage, etc.) before recommending treatments to reduce the risk of the cancer coming back. Axillary lymph node dissection may be recommended.
The study reviewed here suggests that axillary lymph node dissection may not have benefits for many women diagnosed with early-stage breast cancer with cancer in the sentinel lymph node who are treated with lumpectomy and radiation — and that for these women, axillary lymph node dissection shouldn’t be done routinely. This may be especially true for women who will have chemotherapy and/or hormonal therapy after surgery. Still, each woman’s situation is unique. For some women, the advantages of axillary lymph node dissection may outweigh the risks. If your doctor recommends axillary lymph node dissection, you may want to ask your doctor about this study and how the results may apply to your situation. With the most up-to-date information, you and your doctor can make the best decisions for YOU.
You can learn more by visiting the Breastcancer.org Lymph Node Removal pages.
Editor’s note: To make sure that women have the appropriate lymph node surgery, the American Society for Clinical Oncology released guidelines on sentinel lymph node biopsy for people diagnosed with early-stage breast cancer. The guidelines say sentinel lymph node biopsy SHOULD be offered under these circumstances:
- breast cancer in which there is more than one tumor, all of which have formed separately from one another (doctors call these multicentric tumors); these types of breast cancers are rare
- DCIS treated with mastectomy
- women who have previously had breast cancer surgery or axillary lymph node surgery
- women who have been treated before with chemotherapy or another systemic treatment (treatment before surgery is called neoadjuvant treatment)
Sentinel node biopsy SHOULD NOT be offered under these circumstances:
- the cancer is 5 cm or larger or locally advanced (the cancer has spread extensively in the breast or to the nearby lymph nodes)
- the cancer is inflammatory breast cancer
- DCIS treated with lumpectomy
- the woman is pregnant
The guidelines also say:
- Women with negative sentinel node biopsies shouldn’t have axillary node surgery.
- Women with one or two positive sentinel nodes who plan to have lumpectomy plus radiation also don’t need axillary node surgery.
- Women who have one or more positive sentinel nodes and plan to have a mastectomy with no radiation should be offered axillary node surgery.”

