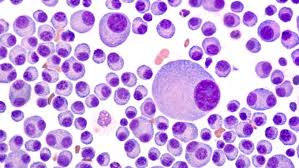
Our results show that thymoquinone (TQ) inhibited the proliferation of MM cells irrespective of their sensitivity to doxorubicin, melphalan or bortezomib.
Multi-Drug Resistance (MDR) is the enemy of all multiple myeloma patients, survivors and caregivers. MM survivors are said to have reached MDR when their multiple myeloma no longer responds to conventional therapies.
Consider evidence-based non-conventional therapies that can, according to research, enhance the efficacy of Velcade aka bortezomib regardless of MDR.
One of the most often asked questions that I receive on PeopleBeatingCancer is if supplement __________ could interfere with chemotherapy ___________. It seems to me that the studies linked below clarify the answer to this question.
Thymoquinone not only does not interfere with Velcade, melphalan and doxorubicin, it can enhance the efficacy of those chemotherapy regimens against multiple myeloma.
- Honokiol, Magnolia Tree Bark- is available on Amazon-
- Thymoquinone, Black Seed Oil- is also available on Amazon-
While I caution all MM patients, survivors and caregivers about the challenges of long-term and/or high-dose toxicity, I have come to view Velcade as being the least of other MM evils.
By this I mean that Velcade has been in clinical practice for more than 10 years. I consider it to be a routine or sort of a backbone MM therapy. Revlimid, Velcade, Dexamethasone is the standard-of-care triplet induction therapy for newly diagnosed MM patients. RVd provides an exceptional overall response rate.
The most popular blog post on PeopleBeatingCancer is about CBD oil enhancing the efficacy of Velcade.
I do not want to come across as a cheerleader for any form of toxic chemotherapy. My point is that the newly diagnosed MM patient must learn about all forms of evidence-based MM therapies including
- Conventional FDA approved therapy
- Integrative Therapy
- Complementary Therapy
To learn more about the spectrum of therapies for multiple myeloma scroll down the page, post a question or comment and I will reply to you ASAP.
Hang in there,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
“Scientists have found a potential new pathway to stop bortezomib resistance in patients with multiple myeloma (MM).
Researchers suggest that strategies could be developed to use BTZ in combination with existing therapies. They additionally note that MM cells produce insulin-like growth factor 1 (IGF-1). BTZ resistance has been associated with heightened levels of IGF-1 and its receptor.
“The IGF-1R inhibitor OSI-906 can increase the cytotoxicity of BTZ in MM cells, and PI3K and AKT are the downstream targets of IGF1,” they write. “AKT inhibition also causes BTZ-resistant cell death,” said the study authors…”
“CONCLUSIONS- A large volume of research in MM has highlighted the cardinal role of the BMME as a complex signaling molecules network, in which MM onset, progression and DR are regulated by a contact-dependent and -independent interplay between MM cells and their surrounding microenvironment. The role of the BMME network has been seen to be more complex since the discovery of the new players, miRNAs, exosomes and CAFs. The therapeutic failure of novel MM agents (first and second generation proteasome inhibitors, IMIDs, etc.) that target cell adhesion, cytokines secretion and survival pathways may be explained by their involvement. Notably, CAFs, miRNAs deregulation and/or the exosomes cargo (miRNAs/cytokines/proteins) could permit MM cells to achieve apoptotic escape and/or prosurvival autophagy by modulating alternative signaling pathways. Nevertheless, in-depth investigations are needed to better elucidate the role of miRNAs, exosomes and CAFs in affecting a tumor-prone BM niche.
In conclusion, MM drug resistance, being a multistep transformation process in which several players cooperate among themselves, provides the rationale for a multiple targets therapeutic approach with the aim of creating an unsupportive BMME and thereby enabling anti-MM therapies.
” Here we show that HNK significantly induces cytotoxicity in human multiple myeloma (MM) cell lines and tumor cells from patients with relapsed refractory MM. Neither coculture with bone marrow stromal cells nor cytokines (interleukin-6 and insulin-like growth factor-1) protect against HNK-induced cytotoxicity.
Furthermore, HNK enhances MM cell cytotoxicity and apoptosis induced by bortezomib. In addition to its direct cytotoxicity to MM cells, HNK also represses tube formation by endothelial cells, suggesting that HNK inhibits neovascurization in the bone marrow microenvironment.
Taken together, our results provide the preclinical rationale for clinical protocols of HNK to improve patient outcome in MM.”
“However, majority of patients with myeloma suffer relapse or develop chemoresistance to existing therapeutic agents. Thus, there is a need to develop novel alternative therapies for the treatment of MM. Thus in the present study, we investigated whether thymoquinone (TQ), a bioactive constituent of black seed oil, could suppress the proliferation and induce chemosensitization in human myeloma cells and xenograft mouse model. Our results show that TQ inhibited the proliferation of MM cells irrespective of their sensitivity to doxorubicin, melphalan or bortezomib.
Interestingly, TQ treatment also resulted in a significant inhibition in the proliferation of CD138+ cells isolated from MM patient samples in a concentration dependent manner. TQ also potentiated the apoptotic effects of bortezomib in various MM cell lines
Overall, our results demonstrate that TQ can enhance the anticancer activity of bortezomib in vitro and in vivo and may have a substantial potential in the treatment of MM.”
“The multiple myeloma drug Velcade (bortezomib) can induce the formation of pro-inflammatory macrophages — a kind of white blood cell — that promote the growth of myeloma tumors…”
Here is the conundrum that all newly diagnosed myeloma patients face. Multiple myeloma drugs such as Velcade are cytotoxic to multiple myeloma (MM). MM toxicity is what causes multi-drug resistance.
According to the study linked below, the more Velcade received by the myeloma patient, the more resistant the MM patient’s blood cancer becomes. Multi-drug resistance (MDR) is only a matter of time.
Multiple myeloma could be managed forever if oncology figured out how to eliminate multi-drug resistance (MDR). Ironically, one of the multiple myeloma drugs given to MM patients that reduces/fights MM also causes inflammation and leads to the very state that triggers end-stage myeloma.
So what is a newly diagnosed MM patient to do?
Full disclosure. My induction chemotherapy regimen VAD did little for me other than cause a series of short, long-term and late stage side effects. I live with a bias against toxic chemotherapy.
My experience combined with the studies below clearly indicate that high-dose, aggressive multiple myeloma drugs cause more problems that it solves. The negatives outweigh the positives.
I believe that newly diagnosed MM patients must walk a fine line when it comes to their incurable blood cancer. Yes, undergo Velcade therapy, but undergo just enough to keep you myeloma under control.
My definition of “under control” is keeping indicators such as your m-spike, free light chains, etc. at a level that is short of causing damage to the patient. In my experience, my version of “under control” is probably more myeloma that what the average oncologist considers “under control.”
Consider-
- Consider thinking about induction therapy with the goal of controlling your MM- don’t have a goal of complete remission…don’t have a goal of completely eradicating all metrics of MM from your body…just control it. Control is preventing your MM from causing damage…
- Consider undergoing evidence-based, non-toxic therapies before, during and after your active therapies. These therapies, according to research, will enhance your immune function, make you stronger and probably make you feel better.
- Consider undergoing evidence-based, integrative therapy shown to enhance the efficacy of Velcade, for example, allowing you to fight your MM with less of the therapy that causes inflammation
- And finally, consider undergoing therapies shown to reduce inflammation, aka anti-inflammatory, that can reduce the inflammation caused by chemotherapy
As a long-term MM survivor, I have come to believe that inflammation and multi-drug resistance are just as much of a problem to the MM patient as his/her MM is. Or at least I should say that the goal of MM therapy should be to fight all three, MM, MDR and inflammation, at the same time.
Recommended Reading:
“The researchers found that treatment with Velcade led to a physiological reaction that actually reinforced the intensity of the myeloma in the mice. According to Prof. Shaked, the drug caused inflammatory cells (macrophages) in the bone marrow to enhance the aggressiveness of the disease and provide the cancer cells with resistance to treatment…
In fact, when the researchers inhibited the secreted factor related to the activity of inflammatory cells, they observed a decrease in the proliferation of cancer cells. Now they are working on various ways to inhibit the body’s response to anti-cancer treatments…”
“The multiple myeloma therapy Velcade (bortezomib) can induce the formation of pro-inflammatory macrophages — a kind of white blood cell — that promote the growth of myeloma tumors, Israeli researchers found.
The presence of such cells in the bone marrow could help explain why some myelomas turn resistant to Velcade. Measuring these cells on marrow biopsies could be used to spot patients who are more likely to become resistant…
Despite its demonstrated benefit in prolonging patients’ survival, some individuals relapse and subsequently develop resistance to Velcade. When this happens, the prognosis is very poor…
Using a combination of human cell lines and animal models, the researchers found that Velcade treatment promotes the enrichment of tumor-initiating cells (TICs), also known as cancer stem cells.
These cells represent a small proportion of cancer cells, but have the ability to self-renew, serving as a storage of cells for tumor initiation and growth.
Specifically, Velcade induced the formation of a type of white blood cells, called macrophages, involved in inflammation. Velcade-treated mice had nearly a 40% increase in the percentage of pro-inflammatory macrophages when compared with mice treated with a placebo.
Such macrophages released factors that promoted the growth of human TICs growing in petri dishes. Consistent with this finding, mice implanted with human myeloma had more TICs in their bone marrow, and lived for a shorter time, after treatment with Velcade.
Further experiments suggested that Velcade drives the expansion of TICs in part due to the release, by macrophages, of interleukin-1-beta (IL-1β) — an inflammatory protein…
Finally, to support the clinical relevance of their findings, the researchers compared cells in bone marrow biopsies of 34 multiple myeloma patients at the time of diagnosis and several months following Velcade treatment.
Confirming their first results, the investigators found more pro-inflammatory macrophages and TICs in the patients’ marrow after treatment with Velcade. An increased percentage of pro-inflammatory macrophages in these patients also was associated with a shorter survival.
“Overall, our results uncover a pro-tumorigenic cross-talk involving pro-inflammatory macrophages and MM cells in response to bortezomib therapy, a process that enriches the MM-TIC population,” the researchers said.
“Based on our findings, we propose that macrophage state and TIC levels in the BM [bone marrow] compartment of newly diagnosed MM patients can be used as a predictive tool for relapse,” they emphasize.
“At present, with the wide repertoire of treatment options for MM patients, it is imperative to incorporate biomarkers that would preclude one treatment modality over the other in clinical decision making,” they added…”