There is no association between conventional response outcomes, such as complete response (CR) or very good partial response (VGPR), and survival in patients with newly diagnosed multiple myeloma-
I am a long-term survivor and cancer coach of a blood cancer called multiple myeloma. The question from Kit below is common. By common I mean that the patient is wondering why he/she should undergo more toxicity if they have already reached remission from their multiple myeloma.
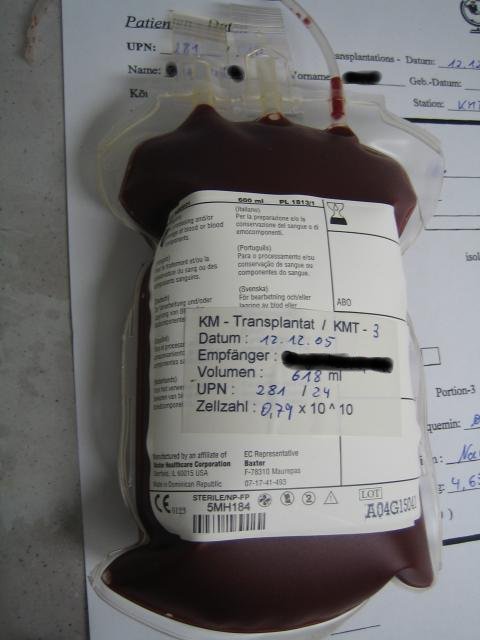
The usual reply given by conventional oncology is that an autologous stem cell transplant (ASCT) is the best option for the patient. The study excerpted and linked below questions why conventional oncology considers an ASCT to be “best.”
According to the article below there is no association between outcomes (CR, VGPR) and survival of patients. In other words, the length of a multiple myeloma patient’s life has nothing to do with achieving a deep remission.
My experience as a multiple myeloma patient is that our mission is to achieve the deepest, longest remissions possible while sustaining the least amount of collateral damage aka side effects.
“From: Kit
Subject: Multiple myeloma stem cell treatment
Hi Cancer Coach:
I was just diagnosed with MM on October 2, 2015. I went through a two cycles of velcade and dexamethasone. Then my doctor added revlimid for a third cycle. I also did a single dose of zometa. I am currently in remission.
My doctors have me scheduled to do a stem cell transplant in the next two weeks. I am concerned about the risks of doing one and wonder if it is truly necessary since I am already in remission.”
To learn more about Stringent or Complete Response click now
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
“There was no association between conventional response outcomes, such as complete response (CR) or very good partial response (VGPR), and survival in patients with newly diagnosed multiple myeloma, according to the results of a meta-regression analysis published recently in the European Journal of Hematology.
“We explored the relationship between response to initial treatment and survival in patients with newly diagnosed multiple myeloma, based on data from 63 randomized clinical trials…” “Meta-regression analyses failed to demonstrate any association between CR or (CR or VGPR) with either overall survival or progression-free survival both in patients receiving autologous stem cell transplant [ASCT] and in non-ASCT patients…”
According to the study, the outcomes of CR and VGPR are commonly used to evaluate the efficacy of treatments for myeloma. However, there are conflicting data on whether or not CR is associated with longer overall and progression-free survival, and the role of transplant in survival outcomes. Instead, newer trials have suggested that the use of minimal residual disease (MRD) status may be a valid surrogate outcomes for survival in patients with myeloma who achieved CR…
Based on the data from these trials, the researchers found no association between overall survival and CR among patients without transplant, in patients who underwent transplant, and in trials comparing transplant with non-transplant patients. Overall survival did not correlate with the combined outcomes of CR and VGPR.
Similarly, an analysis of trials of patient who did not undergo transplant showed no correlation of progression-free survival with CR or with combined CR and VGPR…
“The lack of association between response rates and hard clinical outcomes raises concerns about fast track approval of new drugs, based on results from trials utilizing solely these surrogate markers,” the researchers wrote. “Given the limitations of CR or VGPR to accurately reflect survival in patients with newly diagnosed multiple myeloma, prospective studies should include MRD in addition to conventional response outcomes.”