Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Diagnosis W/ Multiple Myeloma W/ Serious Kidney Involvement-
Diagnosis W/ Multiple Myeloma W/ Serious Kidney Involvement-

“Progression to ESRD was rare, but CKD was common, and longer follow-up may uncover a greater burden of slowly progressive CKD in patients with treated LCPT.”
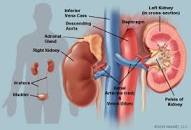
Hi David, I was diagnosed multiple myeloma with light chain proximal tubulopathy (multiple myeloma with extensive kidney involvement) in October. I had been experiencing fatigue for years – but especially in the last 3 years – and pain in my back and hip from Oct. 2018 to Oct 2019 when I was diagnosed. One of the doctors called out my low kidney numbers and told me to go get that checked out – that’s how Mayo Clinic in MN diagnosed the MGRS in late October.
My light chains were 33 – I have no genetic markers that they found – and I don’t even know what the IGA, IGG type numbers mean but I don’t have any of those either.
My bone percentage showed 7-8% MM cells in my bone marrow. No visible bone lesions, but my back and hip pain have almost disappeared since I have been on chemo. Doctors say they don’t suspect bone involvement but I am suspicious since that pain was constant for a year and has now decreased.
I was not taking any supplements because the oncologist said not to take anything during chemo – but after the 4th cycle I started taking fish oil, Curcumin, and b12. I have read about HBOT and wonder if that is something I should try. I started your course but have been overwhelmed and terrified and sort of in a frozen state the past few weeks with my light chain numbers going up.
I feel that the kidney involvement makes my prognosis worse and that is my main fear.
Hi Katherine-
My replies are below…
David Emerson
- MM Survivor
- MM Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Free light Chains and Myeloma Remission/Relapse?
- Multiple Myeloma Chemotherapy leads to Partial Remission”
- Multiple Myeloma Relapse? Dec. M-spike, Inc. Freelight Chains…
Light Chain Proximal Tubulopathy: Clinical and Pathologic Characteristics in the Modern Treatment Era
“Light chain proximal tubulopathy (LCPT) is characterized by cytoplasmic inclusions of monoclonal LC within proximal tubular cells…
Hematolymphoid neoplasms, known before biopsy in only 15% of patients, included:
- 21 monoclonal gammopathies of renal significance;
- 15 multiple myelomas;
- seven smoldering multiple myelomas;
- and three other neoplasms.
Biopsy indications included Fanconi syndrome (38%; all with crystalline LCPT), renal insufficiency (83%), and proteinuria (98%)…
In summary, LCPT presents unusual diagnostic challenges because most patients have no prior history of hematolymphoid disease, intracytoplasmic light chain inclusions may be undetectable by routine immunofluorescence, and crystals may not be visible by LM.
The only independent predictor of final eGFR was initial eGFR, highlighting the importance of early detection.
Most treated patients, including all patients with crystalline LCPT receiving SCT, demonstrated stable or improved kidney function, indicating the benefit of aggressive therapy in selected patients with LCPT.
Progression to ESRD was rare, but CKD was common, and longer follow-up may uncover a greater burden of slowly progressive CKD in patients with treated LCPT.”