I fired Dr. T. and told him that if someone hangs up a shingle as primary care doctor and doesn’t know the symptoms of esophageal cancer, then he shouldn’t be in the business.
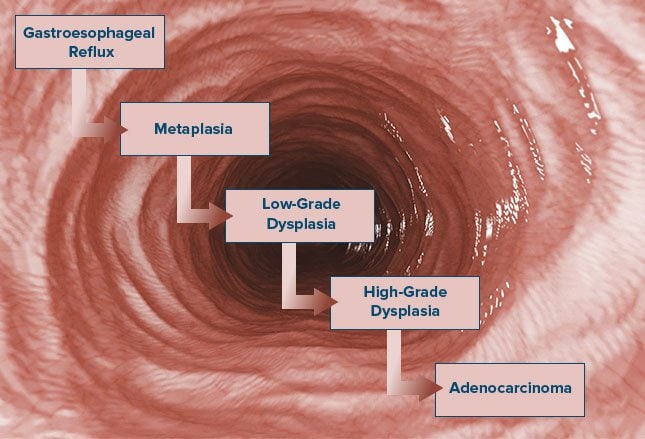
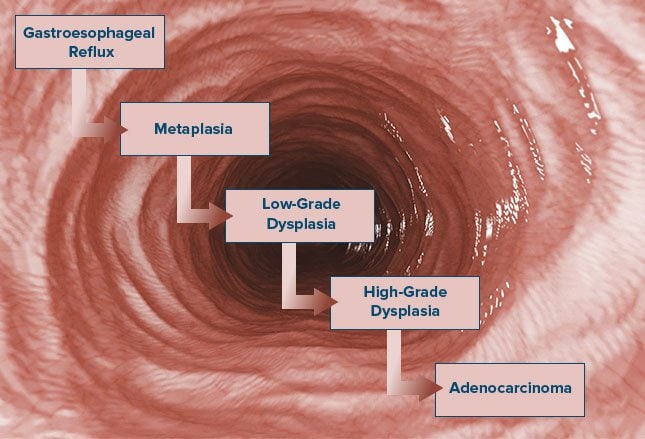
In 1994 I was diagnosed with cancer of the esophagus. This is the story of my diagnosis and treatment. I was born in Fall River, Massachusetts in 1932. From my twenties on, I experienced acid reflux on a regular basis and over the years consumed a lot of Gelusil.
- When I was in my early forties, an esophageal ring was detected at Mt. Auburn Hospital in Cambridge, Massachusetts, but no treatment was prescribed.
- When I turned 60, I began to experience soreness at the sternum radiating up to the neck, with headache.
For 20 months, I called this to the attention of my primary care doctor, a respected cardiologist whom I had been seeing for 15 years — we had served together in the American Heart Association. He x-rayed me, stress-tested me on his treadmill, sent me to a neurologist, but did not refer me to the one doctor who could have detected my esophageal cancer early on, a gastroenterologist. I saw Dr. T, at least six times during those 20 months, complaining each time of the symptoms.
Then, on June 7, 1994, on a business trip to New York City, I collapsed at a restaurant, coughing up blood. An endoscopy at New York University Hospital revealed a “polyp”, and three days later I was sent back to Boston for treatment for esophageal cancer.
The “polyp” turned out to be a cancerous growth of “impressive” size. When Dr. T. (my primary care doctor) gave me the bad news, he reached across his desk to a binder and produced the name of Dr. G., a general surgeon. “Do you know him?” I asked. “No, but he’s in your insurance plan.”
Recommended Reading:
So after Dr. T’s having seen me for 15 years, the best he could do for me in this great center of American medicine was refer me to a general surgeon he didn’t even know. I later fired Dr. T. and told him that if someone hangs up a shingle as primary care doctor and doesn’t know the symptoms of esophageal cancer, then he shouldn’t be in the business.
Most wounding of all was that he didn’t take the time to make a few phone calls to see who was doing the best work in this field in Boston. Dr. T. practiced medicine at its coldest and least caring. He combined incompetence and indifference — a damning combination.
My first visit with Dr. G., the general surgeon, was unsettling. He appeared to be a few years older than me, and he drew sketches on the paper of the examining table of how he might open me up. He didn’t seem to be too sure about the best way to do this surgery. He sent me to Beth Israel for x-rays and CT- scans.
At Beth Israel Hospital two days later, after my CT-scan, I bumped into Dr. G. in the hallway and asked if he had seen my x-rays and if we could put a team of people together: an oncologist, a gastroentrologist, and himself to discuss my treatment. “You can do that if you want,” he said, as we stood in the hallway, surrounded by people. “But it won’t make any difference. Your chance of survival is not very good — only 10%. This is a very bad type of cancer.” In my mind, in that instant, I fired Dr. G. Luckily, from the moment I came back to Boston, I had been on the phone calling everyone I knew for references to doctors in Boston who were treating my type of cancer. One name kept coming up over and over again: Dr. John Wain, a thoracic surgeon at the Massachusetts General Hospital.
As fate would have it, my younger sister, Mary — a nurse in Fall River — was taking a course with a personal friend of Dr. Wain. He insisted on making an appointment for me with Dr. Wain. So after my corridor encounter with the general surgeon, I went directly to Mass General and saw Dr. Wain. He looked at my x-rays and CT-scans and confirmed the diagnosis. He said that the protocol they were using (two months chemotherapy followed by surgery) was producing good results.
“Is your 5-year survival better than 10%?” I asked. “We’re getting about 50% survival for five years,” Dr. Wain said. “I’ll take it,” I said. So he sent me down to talk to Dr. Robert Carey, an oncologist. The next day I started my chemotherapy. It was easier than I anticipated, despite the hair loss and other side effects. During this time I drove out to Lancaster, Massachusetts, to consult with the medical director of the Ayurvedic Health Center. I began a regimen of daily self-administered full-body massages, the taking of certain herbs, drinking a lot of warm water, and eating rather strictly. I had been meditating for 20 years, so daily meditation was nothing new.
My sister Dorothy sent me audio tapes of Dr. Richard Moss that were very helpful. I also began to listen to classical music in a new way — letting the music wash over me uncritically. I also went for a weekly massage, believing that this was a way of stimulating my immune system and getting rid of some of the toxins of chemotherapy. I took money out of my pension fund to pay for this, figuring that if I didn’t survive, I wouldn’t need the pension anyway.
The chemotherapy itself was uneventful except for an allergic reaction to one of the drugs, which drug was promptly suspended. I was hoping that the chemotherapy would shrink the tumor, but a pre-surgery scope didn’t show any serious shrinkage. I prepared for surgery.
I met with Dr. Wain a week before surgery and asked him not to have others in the operating suite who were not required and not to have interns do any of the surgery, except perhaps the opening and closing. He agreed. I had some medical tests the day before surgery and met with the anesthesiologist, who described my pending surgery as “formidable.” He explained that I would be opened up in two places and that the surgery would last about 7 hours.
That night, I finalized my will and wrote a letter to my daughters “to be opened in the event of my death.” My sister Dorothy (an angel) and her husband Dor drove me to Mass General at 5:00 a.m. the next morning and waited there with Jennifer, my older daughter) until I came out of surgery in the late afternoon. The surgery took 9 hours, and I was later told by the nurses that Dr. Wain never left the room. God bless him! My recovery was very slow.

The first tests of liquids never got through the pyloric valve. So they brought me back to surgery to dilate the pyloric. Eventually, I was able to tolerate liquids, apple sauce, sherbet. On one of those dreaded forced marches up and down the hospital corridor, I met my oncologist. “Well, you’re a lucky man,” he said. “We examined 19 lymph nodes and none of them had cancer. So at this moment you are cancer free.”
To tell you the truth, I was feeling so miserable, I didn’t really care. I found out later that my tumor staging was T3, NO, MO. It was adenocarcinoma arising in Barrett’s esophagus. The surgeon had removed 1/2 of my esophagus and 1/3 of my stomach, and my new stomach was now sitting right in the middle of my chest, over to the right.
After two weeks in the hospital, I was discharged and went to live with my sister Dorothy for two weeks. (After 20 years of marriage, I separated in 1990 and divorced in 1994.) My energy was low and I was able to eat very little. I was getting most of my nourishment from a j-tube.
I slept in a hospital bed (provided by PruCare Insurance), but usually got up at 3:00 a.m. and sat in a chair for the rest of the night. At the end of two weeks with Dorothy, I decided to go back to my apartment. Not a good idea! It was difficult taking care of myself, especially the feeding part. I was barely able to move out of my chair most of the time.
Finally, after two weeks, I came down with pneumonia and was taken back to Mass General by ambulance, where I stayed for another two weeks. During this time, I became depressed, a condition I had never before experienced. When I asked for medication for this, two bearded psychiatrists examined me and prescribed a mild heart stimulant, which seemed to do the trick. I stayed on it for about a week.
It was now the middle of October. My surgery had been on August 28th. My voice was weak, probably from the intubation. (In time, it returned to its regular strength.)
From Mass General I went by ambulance to Youville Rehab Hospital since my doctors weren’t going to risk my trying to make it on my own again. I spent two and 1/2 weeks there — and it was great. A lot of physical therapy, spiritual counseling, excellent nursing, good food, and a wonderful environment.
I was released on November 4, 1994, just in time to vote. I didn’t go back to work for the rest of November, trying to eat difference foods each day, and remembering which ones were best for me. The j-tube stayed in. I was growing to hate Ensure, which I was taking by tube and in three glasses a day.
I felt no hunger or appetite but ate by the clock. Many times after eating, I would get a feeling of seasickness, which usually passed in about 45 minutes. My energy level was poor, but I forced myself to do daily physical exercises. I didn’t get back to meditating for a long time and I fell away from my Ayurvedic practices.
Three months after surgery, I started to drive my car again and went back to work in late November. I left work at 3:00 each afternoon, since I ran out of energy by that time of the day. Three months later I traveled to New York City on company business and did very well.
If there is any advice I can give you it is HANG IN THERE. My life was pretty miserable from the time of my surgery for about three months. But now it is not very different from what it was before. True, I have a little less energy, eat smaller meals, and take medication to combat the reflux.
Occasionally, I also suffer from the “dumping syndrome,” which happens to those who have had stomach surgery. But life is sweet. And I can honestly say that I have never enjoyed it more!
Steve Dunn’s CancerGuide, which I discovered when I bought a computer during my chemotherapy, has been a godsend to me. Oncolink and Medline and the National Medical Library are great — but Steve’s personal touch and extremely useful information have meant more to me than any other source.
Somewhere in the Bible it is written that, “those who instruct many will shine as the stars for all eternity.” In my book, Steve Dunn is already one of those stars. Bravo, Stephen!
Update: February 2009 It is now over 14 years since my diagnosis of esophageal cancer. For the longest while after surgery, I experienced discomfort after eating, a feeling of being seasick that lasted about 45 minutes. I now avoid this feeling by not drinking liquids with the meal. I have also learned to eat much smaller meals.
I take one 20 mg Prilosec daily to prevent reflux. I was able to work full time until I retired in the summer of 1999, can eat any type of food, drink alcohol, sleep through the night (in a recliner), and have very few side effects from my former cancer.
I lost 40 pounds after the surgery but gained 20 of those back, which now puts me at my ideal weight. I no longer see my oncologist. I consider myself blessed by the gift of these extra years and count every day a miracle.
I have renewed lost friendships, enjoy the company of my two daughters and three grandchildren, and value the preciousness of life. I have been on two trips to Italy, in 1997 and 2000. Retired from my work with the U.S. Fund for UNICEF, now at the age of 77, I am busy with writing, photography, consulting, web page design, visiting family and friends, and enjoying life more than ever before.
I hope that my story has been helpful. If anyone wants to contact me, I can be reached at ejmitch32@gmail.com. Since first posting my story in CancerGuide, I have heard from hundreds of people around the world and have answered every one of them. I wish you health and happiness.