
Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- End-Stage Multiple Myeloma- Magic Mushrooms?
End-Stage Multiple Myeloma- Magic Mushrooms?
“Therefore, it is not surprising that patients may experience a diagnosis of cancer as sudden, catastrophic, and/or life-threatening.”
Not all cancer diagnoses are alike. I’m not minimizing the seriousness of a cancer diagnosis. I’m saying that a diagnosis of end-stage multiple myeloma is fundamentally different than a diagnosis of a type of cancer that is curable. Consider Psilocybin as therapy.
While I’ve often written about the negative emotions that can accompany living with multiple myeloma, I hadn’t given much thought to possible therapies that may treat these negative emotions. Let me be specific.
When I was first diagnosed with MM, I was full of hope. I think a lot of newly diagnosed MM patients are. I often read people say things like “I’m going to beat this thing.”
Yes, I was told that the average life expectancy of a MM patient was 3-5 years but I was hopeful at the same time. After all, my oncologist used phrases such as
Being relatively young (34) when I was first diagnosed, I thought I had a real shot at curing my MM. If I knew then what I know now…
When I launched PeopleBeatingCancer in June of 2004 I began researching many of the central issues that face a multiple myeloma survivor. I came to understand that there were no documented cases of conventional therapies curing multiple myeloma. I read studies documenting advancements in remissions. I read about increases in OS aka overall survival. But conventional oncology, as far as I found, had never cured multiple myeloma.
I don’t remember when but I stumbled on to a study documenting PTSD in cancer patients. Some studies, like the one linked and excerpted below, explained that a diagnosis of PTSD may occur in cancer patients general.
I read one study that documented PTSD due to aggressive therapy such as a hematopoietic stem cell transplantation (HCT). I underwent an autologous stem cell transplant in 12/95.
We can debate the pros and cons of surgery, radiation and chemotherapy for MM patients and survivors but the fact is, by not being able to cure MM, patients and survivors of MM suffer psychologically.
Whether that suffering is called PTSD or MM survivors are simply understood to be psychologically damaged, the fact remains that MM and it’s standard-of-care therapies cause end-stage multiple myeloma survivors a world of hurt.
According to the second article linked below, psilocybin aka magic mushrooms, may be a possible therapy for the negative emotions experienced by end-stage multiple myeloma survivors. No, magic mushrooms won’t cure end-stage multiple myeloma. But magic mushrooms may provide a reduced sense of “demoralization, hopelessness and death anxiety” to end-stage multiple myeloma survivors.
Are you facing end-stage multiple myeloma? To learn more, scroll down the page, post a question or comment and I will reply to you ASAP.
Hang in there,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Multiple Myeloma Diagnosis – A How-To Guide
- Multiple Myeloma Symptom, Side Effect- Renal Insufficiency, Kidney Failure
- Baking Soda, Curcumin, Doxorubicin as Integrative Multiple Myeloma Therapy
Psilocybin
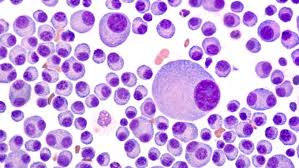
“Psilocybin[a] (/ˌsaɪləˈsaɪbɪn/ sy-lə-SY-bin) is a naturally occurring psychedelic prodrug compound produced by more than 200 species of mushrooms, collectively known as psilocybin mushrooms.
In general, the effects include euphoria, visual and mental hallucinations, changes in perception, a distorted sense of time, and spiritual experiences, and can also include possible adverse reactions such as nausea and panic attacks…”
Long-Term Improvement in Distress Achieved With Psilocybin in Patients With Life-Threatening Cancer
“Psilocybin-assisted psychotherapy appeared to be associated with long-term reductions in distress among patients with life-threatening cancer (multiple myeloma)…
In this crossover study, patients (N=29) who had psychiatric distress in connection with cancer initially received either a 0.3-mg/kg dose of psilocybin or 250 mg of niacin as a control. At a second session, patients switched treatments, so that each patient ultimately was given a single dose of psilocybin. All patients additionally received psychotherapy. The study included 2 long-term follow-ups that were analyzed for this report…
At the 4.5-year follow-up, 57% of patients had clinically significant anxiolytic responses. Clinically significant antidepressant responses were reported for 57% to 79% of patients, depending on the screening tool used for analysis. In an analysis that considered anxiety and depression together, clinically significant responses were seen in 71% of patients. Improvements were also prominent in areas of demoralization, hopelessness, and death anxiety…
All participants at the 4.5-year follow-up indicated they had experienced a positive behavioral change related to the psilocybin treatment. Most patients also considered this treatment to have provided an experience that was spiritually significant, personally meaningful, and/or a contributor to well-being or life satisfaction.
The researchers noted that the study’s crossover design may constrain interpretations, but in their report they wrote that “the treatment continues to be associated with reductions in anxiety, depression, hopelessness, demoralization, and death anxiety up to an average of 4.5 years following a single psilocybin session in conjunction with psychotherapy.”
CALM: A Depression Intervention for Cancer Patients at the End of Life
“The Managing Cancer and Living Meaningfully (CALM) intervention effectively relieves and prevents depression among patients with advanced cancer at the end of life compared with usual care…
Evaluations of patients who underwent CALM — a supportive-expressive psychotherapeutic intervention — revealed improvements in depression, death anxiety, spiritual well-being, and attachment security, but findings were qualitative; quantitative results were previously not ready for analysis…”
Are we missing PTSD in our patients with cancer? Part I
“Posttraumatic Stress Disorder (PTSD) can be defined by the inability to recover from a traumatic event…
A common misconception is that PTSD can only develop in circumstances of war or acute physical trauma. However, the diagnostic criteria of PTSD were adjusted in the Diagnostic Statistical Manual of Mental Disorders Fourth Edition (DSM-IV) to include the diagnosis and treatment of a life-threatening illness, such as cancer, as a traumatic stressor that can result in PTSD.
The word ‘cancer’ is so strongly linked to fear, stigma, and mortality, that some patients are fearful to even say ‘the C word’.
Therefore, it is not surprising that patients may experience a diagnosis of cancer as sudden, catastrophic, and/or life-threatening. Cancer-related PTSD (CR-PTSD) can negatively affect a patient’s psychosocial and physical well-being during treatment and into survivorship. Unfortunately, CR-PTSD often goes undiagnosed and, consequentially, untreated.



