Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- diagnostic testing »
- Enhanced Cystoscopy for Early Bladder Cancer
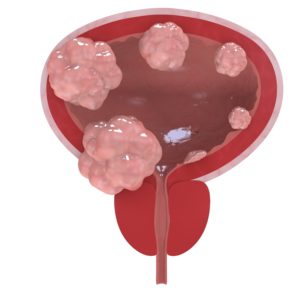
Enhanced Cystoscopy for Early Bladder Cancer

Blue Light Cystoscopy (BLC) increases detection rates of carcinoma in-situ and papillary lesions over WLC alone and can change management in 14% of cases…
Imagine that you are a newly diagnosed bladder cancer patient. You are trying to figure out if you should get a second opinion. Further, you want to make sure that your original diagnosis was accurate aka they doctor identified all possible bladder cancer tumors. Think- what did your doctor use for the cystoscopy?
The article and study linked and excerpted below say that blue light cytoscopy combined with white light cytoscopy catch more NMIBC’s than white light cytoscopy alone.
If your urologist didn’t add blue light cytoscopy to the analysis of your bladder then he/she might have missed spots that may relapse in the coming months or years. Combining both BLC and WLC catches more possible cancer.
Lastly, you can include foods, nutritional supplements and lifestyle therapies that research has shown can reduece your risk of bladder cancer relapse.
I am a cancer survivor and cancer coach. Have you been diagnosed with NMIBC? Scroll down the page, post a question or comment and I will reply to you ASAP.
Thank you,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Muscle-Invasive Bladder Cancer- Integrative Chemotherapy
- Robotic vs Open Cystectomy in Bladder Cancer?
- Curcumin, Green Tea Extract Enhance BCG for Bladder Cancer
Enhanced Cystoscopy Improves the Care of Bladder Cancer Patients
“Depending on the grade and stage at initial diagnosis, up to 61% of patients with Non-Muscle Invasive Bladder Cancer (NMIBC) will experience recurrence within the first year after initial resection, and up to 78% will experience recurrence within five years.
In addition, there is a high risk for progression to muscle-invasive bladder cancer, with approximately 17% of patients progressing at one year and 45% progressing at five years. Thus, the journey of patients with NMIBC is frequently characterized by multiple tumor recurrences and repeated therapeutic interventions over the course of their care, typically requiring lifelong monitoring. These statistics help to explain why bladder cancer is one of the most expensive cancers to manage, accounting for almost $3.7 billion in direct costs in the US each year…
Recently updated clinical practice guidelines (April 2016) that include a joint effort between the American Urological Association (AUA) and the Society of Urologic Oncology (SUO) provide guidance for improving bladder cancer care by
- emphasizing that early and accurate diagnosis,
- proper risk stratification, and
- precise and thorough resection of the tumor before other treatments are started are paramount in the care of patients with NMIBC…
Importantly, the clinical guidelines also provide evidence for other factors that predict for a high-risk of progression, including:
- lymphovascular invasion,
- prostatic urethral involvement,
- variant histology,
- any carcinoma in situ (CIS) and
- poor response to bacillus Calmette-Guérin (BCG) intravesical therapy…
Specifically, the guidelines state that clinicians should offer blue light cystoscopy (BLC), if available, as an adjunct to traditional white light cystoscopy (WLC) to increase tumor detectionand decrease recurrence and improve staging and risk stratification. An estimated 10% to 20% of bladder tumors are missed using traditional WLC alone, and 34%-76% of patients have evidence of residual tumor on repeat TURBT 2-6 weeks later...”
Blue light cystoscopy for the diagnosis of bladder cancer: Results from the US prospective multicenter registry.
“Results- Overall, 1,632 separate samples from bladder resection or biopsy were identified from 641 BLC procedures on 533 patients: 85 (16%) underwent repeat BLC (range: 2-5). Sensitivity of WLC, BLC, and the combination for diagnosis of any malignant lesion was 76%, 91%, and 98.5%, respectively. Addition of BLC to standard WLC increased detection rate by 12% for any papillary lesion and 43% for carcinoma in-situ. Within the WLC negative group, an additional 206 lesions in 133 (25%) patients were detected exclusively with BLC. In multifocal disease, BLC resulted in AUA risk-group migration occurred in 33 (6%) patients and a change in recommended management in 74 (14%). False-positive rate was 25% for WLC and 30% for BLC. One mild dermatologic hypersensitivity reaction (0.2%).
CONCLUSIONS- BLC increases detection rates of carcinoma in-situ and papillary lesions over WLC alone and can change management in 14% of cases. Repeat use of HAL for BLC is safe.”