Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Exercise-Based Cardiac Rehabilitation
Exercise-Based Cardiac Rehabilitation
(HF) Patients assigned exercise-based cardiac rehabilitation had greater improvements in exercise capacity and health-related quality of life compared with those assigned the control…
I’m a long-term survivor of an incurable blood cancer called multiple myeloma. Out of nowhere, I developed a late stage side effect. After about 15 years of normal heart function,
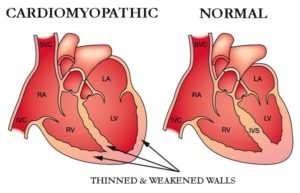
In December of 2010, I was diagnosed with chemotherapy-related cardiomyopathy (CRC), sometimes called chemotherapy-induced cardiomyopathy (CIC). Cardiac Rehab is now my daily priority…
I’m writing both terms because I don’t know which phrase is more accurate. The goal of this post is to tell all multiple myeloma survivors that CIC or CRC may be a part of their future.
I also know that I want nothing to do with toxic medications. I experienced almost four years of toxic hell when I underwent induction chemotherapy and an autologous stem cell transplant for my newly diagnosed multiple myeloma. Never again.
I learned that quantifiable progress could be made in both my general health, maintaining multiple myeloma remission and heart health in this case, through evidence-based, non-toxic therapies. In the case of the studies linked and excerpted below, frequent, moderate exercise.
I’m not talking about workouts that exhaust you. After all, I have cardiomyopathy. I’m talking about frequent moderate exercise to lower blood pressure the natural way. I’m on an elliptical several mornings each week and I lift light weights on the other mornings.
I understand that some multiple myeloma/ cardiac rehab patients want to go to a specific facility and work with people with degrees in heart health. That’s fine.
I’m documenting those evidence-based, non-toxic therapies that have helped my manage my CIC since late 2010. I’m talking about:
- exercise (moderate, daily, cardio and weight-bearing)
- nutrition, (the Mediterranean Diet, nuts, a bit of wine…)
- heart healthy supplements (CoQ10, PQQ, Mag. more) and
- other heart healthy complementary therapies.
The pay off? According to research chemotherapy-induced cardiomyopathy has a 10 year life expectancy. As of the writing of this post, not only have I lived more than 10 years, my ejection-fraction has improved by 25%, my weight has been stable, my BP has been stable and I feel great!
To learn more about surviving multiple myeloma and about evidence-based, non-toxic heart therapy, scroll down the page, post a question or comment and I will reply to you ASAP.
- Learn more about chemotherapy-induced cardiomyopathy- click now
- To Learn More about Exercise Enhancing Overall Survival- click now
Thank you,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer.org
Recommended Reading:
- Cardiac Rehabilitation-Curcumin, Cardiovascular Disease, Heart Failure
- Heart Failure + Surgery = Higher Risk of Death
- Home-Based Cardiac Rehabilitation- Evidence-based but Significantly Underused
Blended treatment for depression, heart failure improves quality of life
“Care composed of treating depression and HF may improve health-related quality of life in the 12 months after hospitalization, according to Hopeful Heart trial findings presented at the American College of Cardiology Scientific Session….
Heart failure is super common in the United States and worldwide,” Rollman said during the presentation. “There’s been a number of studies that show that depression is highly comorbid in hospitalized heart failure patients and is also associated with decreased health-related quality of life, decreased adherence with evidence-based care, increased mortality, readmissions and health care costs…””
Exercise-based cardiac rehab confers improvements in HF
“Exercise-based cardiac rehabilitation in patients with HF resulted in improvements in exercise capacity and health-related quality of life compared with patients who did not exercise, according to a study published in the Journal of the American College of Cardiology…
“These results, based on an [individual participant data] meta-analysis of randomized trials, support the class I recommendation of current international clinical guidelines that [exercise-based cardiac rehabilitation] should be offered to all HF patients and the need to improve current poor uptake of [exercise-based cardiac rehabilitation] in this population…”
Researchers analyzed data from 3,990 patients with HF (97% with HF with reduced ejection fraction) from 13 trials included in the ExTraMATCH individual participant data meta-analysis. Trials were included in this study if they were randomized with patients with HFrEF or preserved ejection fraction, exercise-based cardiac rehabilitation for a minimum of 3 weeks, a comparator arm that was not assigned exercise intervention…
Patients assigned exercise-based cardiac rehabilitation had greater improvements in exercise capacity and health-related quality of life compared with those assigned the control…
Exercise training in cancer related cardiomyopathy
“Besides classical symptoms of heart failure with or without decompensation, an overwhelming majority of cancer patients develop fatigue and a significant reduction in exercise capacity when compared to their pre-cancer state. These effects seem to be independent from the specific chemotherapeutic substance included in the treatment regimen.
Recent trials have suggested beneficial effects of exercise regiments in early and late phases of cancer treatment regimens and during rehabilitation. This review focuses on the currently available literature and evidence for the role of exercise training in preventing declining cardiac function or improving an already impaired function during or after chemotherapy, radiation or other cancer-specific therapies…
One of the biggest issues due to its mortality-defining nature is the wide range of cardiac and cardiovascular toxicities affecting the entire cardiovascular-skeletal muscle axis (2,3)…
One of the worst complications of chemotherapeutic treatments is the development of chemotherapy-related cardiomyopathy (CRC) which can develop years if not decades following the initial treatment.
The mortality rate in cancer survivors with cardiomyopathies is significantly higher than for idiopathic non-ischemic cardiomyopathy. A study in 2000 found a 3.5-fold increase in mortality for doxorubicin induced cardiomyopathy compared to idiopathic non-ischemic cardiomyopathy…
Moreover an overwhelming amount of cancer survivors suffer from a reduction in quality-of-life related to symptoms of fatigue, nausea, pain and depression occur frequently. Studies also show that exercise capacity as measured in cardio-pulmonary exercise testing is reduced in approximately 70% of cancer patients (10)…
This review focuses on the currently available evidence for the role of exercise training in preventing declining cardiac function or improving an already impaired function during or after chemotherapy, radiation or other cancer-specific therapies…
Cancer-related cardiomyopathy (CRC) is a condition with very heterogeneous underlying pathomechanisms due to the varying modes of action of the suspected causing drug (11).
Ewer and Lippman introduced a general classification in 2005 which is based on the presence or absence of structural abnormalities and the extent of functional reversibility. Subsequently CRC is classified in an injury type with permanent loss of function (Type 1) and a dysfunction type with temporarily and often reversible loss of cardiac function (Type 2) (12)…
The list of drugs suspected or proven to cause CRC is long and probably growing with the continuing introduction of modern novel therapy protocols. One of the best studied and well-established drugs classes are probably anthracyclines usually causing permanent structural changes. Also anthracycline induced CRC is occurring quite frequently and is usually associated with a poor prognosis (16,17). Among other substance classes that can cause structural cardiac impairment are high-dose alkylating agents and small-molecule tyrosine kinase inhibitors (18)…
The recent addition of checkpoint inhibitors targeting CTLA-4 (ipilimumab), PD-1 (nivolumab and pembrolizumab) and PD-L1 (atezolizumab, durvalumab, avelumab) show also next to promising results in cancer therapy a significant rate of cardiotoxic side effects...
- Exercise training before cancer therapy
- Exercise training during cancer therapy
- Exercise training after cancer therapy
Conclusions
As of today there is only limited evidence that exercise therapy can actually prevent or mitigate CRC. However, there is plenty of evidence to support the importance of exercise in cancer treatments in order to improve cardio-respiratory fitness of patients during and after cancer treatment.
This significantly improves typical treatment associated symptoms such as fatigue which is an important end-point for patients and physicians alike. However, it cannot be a suitable surrogate parameter for actually improving cardiac function or decreasing cardiovascular mortality…”