
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Fatal Adverse Events AKA Death from Immunotherapy Drugs
Fatal Adverse Events AKA Death from Immunotherapy Drugs
Given the increasing use of immune checkpoint inhibitors (ICIs), a concomitant rise in adverse events is inevitable…We found the staggering difference of incidence of fatal adverse events (FAEs).
Fatal adverse events. Serious but relatively rare. If you’re like me, you might toss off this risk thinking that it can’t happen to you. Or, you might think that your primary concern is to control your cancer first and worry about side effects later. But according to the studies linked below, FAE’s, cardiotoxicity (heart damage), eyesight damage and hemotological (blood) risks are real and potentially serious. What if you could have your cake and eat it too?
Twenty-five years of surviving an incurable cancer has taught me that side effects like FAEs, cardiotoxicity, and hematological (blood) problems are not a zero-sum, all or nothing equation. Experience has taught me that the cancer patient can reduce his or her risks of the negative aspects of toxic therapies through personal effort. When I say personal effort, I’m simply talking about what we patients can do on our own.
Research as also shown that cancer patients do better when they pre-habilitate.
Therefore a cancer patient considering immunotherapy might be able to improve his/her chances of avoiding a fatal adverse event by pre-habiliating. I can’t cite studies that support this idea but I’m posting a blog about this possible therapy because the degree of all types of adverse events caused by immonotherapies is staggering.
- To Learn More about the Harmful Effects of Immunotherapy- click now
- To Learn More about the pros and cons of immunotherapy- click now
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Head & Neck Cancer-Pembrolizumab Treats Relapsed Patients
- End-of-Life Mind-Body Therapy for Advanced Cancer Patients
- Carfilzomib-Induced Heart Damage in Multiple Myeloma
Risk and incidence of fatal adverse events associated with immune checkpoint inhibitors: a systematic review and meta-analysis
Background: Given the increasing use of immune checkpoint inhibitors (ICIs), a concomitant rise in adverse events is inevitable. In a recent Phase III trial of ICIs versus placebo, we found the staggering difference of incidence of fatal adverse events (FAEs). Hence, we should determine the risk of FAEs in ICIs.
Methods: Literature searching was based on PubMed before April 15, 2018. The numbers of FAEs in both study group and placebo group were collected. We assessed the risk of fatal adverse reactions associated with ICIs on Pooled Peto OR and associated 95% CI.
Results: Twelve trials were identified. OR value of FADs in all ICIs was 2.32 (95% CI: 1.33, 4.05; P=0.003). The incidence of FAE in ICI in all included studies were up to 3.2%. OR value of clinical trials of prostate cancer was 3.71 (95% CI: 1.12, 12.26; P=0.03). Among the ICI cohorts, the common FAEs were gastrointestinal toxicity (n=12, 25%), pulmonary toxicity (n=10, 20%), cardiac toxicity (n=5, 10%), and hepatic toxicity (n=5, 10%).
Conclusion: The cytotoxic T-lymphocyte-associated protein-4 (CTLA-4) inhibitors have a significantly higher risk of FAE (P=0.01), whereas programmed cell death protein 1 (PD-1) inhibitors were not. The most common CTLA-4-related FAE was gastrointestinal toxicity, and the most common PD-1-related FAE was pulmonary toxicity. Moreover, we have shown that ipilimumab has significant dose-dependent lethal toxicity.
Checkpoint Inhibition and Cardiotoxicity: Cause for Concern?
“An extensive analysis of a World Health Organization (WHO) global database has identified
as significant immune-related cardiac toxicities associated with the use of immune checkpoint inhibitors (ICIs) in routine clinical practice.
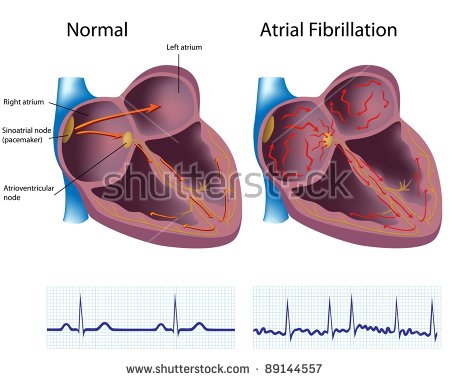
These cardiotoxicities were seen more often in men than women. Pericardial diseases were more common in patients with lung cancer (56%), whereas myocarditis (41%) and vasculitis (60%) were more common in patients with advanced melanoma. Death resulting from myocarditis, pericardial disease, and vasculitis was reported to occur in 50%, 21%, and 6% of patients, respectively. Importantly, many of these events occurred early in the course of treatment with ICIs.
The study, which was published online November 12 in Lancet Oncology, is an extension of earlier published correspondence, which was reported by Medscape Medical News…
Adverse events caused by nivolumab and ipilimumab can be sight-threatening
“This is the largest case series assessing ocular immune-related adverse events (IRAE) in patients treated with immunotherapy agents nivolumab and ipilimumab-
Outcomes- Fifteen patients (1%) developed immune-related adverse events. Metastatic cutaneous melanoma was noted in 12 patients; 2 were cases of uveal melanoma and 1 was a non-small-cell lung carcinoma.
Researchers observed ocular toxicities such as ocular myasthenia, corneal punctate epithelial erosions, subconjunctival hemorrhage, corneal perforation, uveitis, hypotony maculopathy, cystoid macular edema, serous retinal detachment, choroiditis, Vogt-Koyanagi-Harada-like syndrome, optic neuritis and melanoma-associated retinopathy. This is the first report of optic neuritis as an IRAE associated with immunotherapy.
Clinical significance- The development of effective immunotherapy is one of the most significant recent advancements in oncology and its use is becoming more widespread. It is important that ophthalmologists recognize and treat potential ocular side effects associated with these drugs.
Hematological adverse events with PD-1, PD-L1 inhibitors warrant better management
“Hematological immune-related adverse events associated with PD-1 or PD-L1 inhibitors, such as neutropenia and hemolytic anemia, are rare but potentially fatal and warrant earlier detection and better management, according to a descriptive observational study published in The Lancet Hematology…”
Exploring Cutaneous Adverse Effects of Immune Checkpoint Inhibitors
“Chemotherapeutic agents have long been linked with adverse cutaneous reactions, including hyperpigmentation, alopecia, photosensitivity, extravasation, palmar-plantar erythrodysesthesia, nail changes, and radiation recall reactions.1 As with traditional cancer therapies, newer treatments have also been found to increase the risk for a range of adverse events.
Since 2011, several immune checkpoint inhibitors have received approval from the US Food and Drug Administration for the treatment of advanced melanoma, beginning with ipilimumab, an anticytotoxic T-lymphocyte-associated protein 4 agent.2 Two anti-programmed cell death protein 1 (PD-1) inhibitors, pembrolizumab and nivolumab, were approved for the same indication in 2014, followed by combined treatment with nivolumab and ipilimumab in 2015…
Immune-Related Adverse Events (irAEs)
Although these agents have shown considerable efficacy and an overall favorable safety profile,3 there have been numerous reports of adverse events affecting nearly every system in the body.2 These include
- cutaneous,
- neurologic,
- ophthalmologic,
- respiratory,
- hematologic,
- cardiac,
- genitourinary, and
- musculoskeletal adverse events
that range from mild to severe, with some cases resulting in death.2
Previous findings indicate that cutaneous immune-related adverse events (irAEs) occur in approximately 40% of patients treated with these medications and these are the most commonly reported type of side effect resulting from the use of immune checkpoint inhibitors.2,4 “
Some of the skin conditions that we see frequently with immunotherapy agents include lichenoid dermatitis, vitiligo, bullous pemphigoid, eczema, and psoriasis,” Dr Chu told Dermatology Advisor…”



