Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Has My Acid Reflux Become Barrett’s Esophagus or EC?!
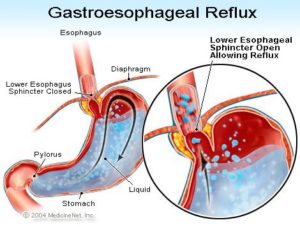
Has My Acid Reflux Become Barrett’s Esophagus or EC?!

It is my recommendation that referral for endoscopy in a patient with suspected GERD (acid reflux) should be reserved for patients with symptoms of GERD who also have alarm symptoms
Hi David, I have been battling with stomach ulcers and acid reflux for 8 years. Had many tests done to rule out Hernias, H Pylori bacteria etc etc. Went from being told I had high stomach acid to low stomach acid and still nothing.
I eat very healthy. Don’t drink, never smoked. I run 5kms a day and believe I am generally in good health. I never take medication as I believe we can heal ourselves but I need all the help I can get….
I am worried my throat is at the stage it could become cancerous and would like to fix it please help me!
Hi Ronda-
I am sorry to read of your acid reflux issues. First and foremost, I am convinced that your diet and lifestyle benefit your health in many different ways. All good.
With respect to your acid reflux, I will reiterate the therapies discussed in the blog post that you came in on, curcumin and omega-3 fatty acids and again, as the post discussed, radiofrequency ablation if your acid reflux has progressed to Barrett’s Esophagus.
This is a bit backwards, but you can undergo an endoscopy (see the article linked below).
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Heal Barrett’s Esophagus, GERD and Eliminate Risk of Esophageal Cancer
- I have Barrett’s Esophagus- what are my options?
- My Dr. told me that this Barrett’s Esophagus leads to Esophageal Cancer- “nasty and has a low cure rate”
- Stage 4 Esophageal cancer with Liver Mets
When Should Endoscopy Be Done in the Patient With Reflux?
“Historically, subspecialists have often depended on objective diagnostic tests in the initial management of disease processes (ie, gastroenterologists would use a test such as endoscopy to diagnose gastroesophageal reflux disease [GERD]), whereas primary care physicians (PCPs) have often relied on clinical findings or the results of trials of empirical therapy to make a disease diagnosis.
This disparity in initial clinical approach in GERD management between specialist gastroenterologists and PCPs is now especially questionable, given that community-based studies have shown that 40% to 60% of patients with reflux symptoms have no objective endoscopic findings of GERD.[1]
Thus, endoscopy only has a sensitivity of approximately 50% for diagnosing GERD. It is my opinion that this relatively modest (at best) sensitivity for endoscopy as a diagnostic test for GERD is underappreciated by many PCPs referring patients with suspected GERD for this procedure as a diagnostic tool.
Furthermore, the charges for upper gastrointestinal tract endoscopy and the additional hidden costs (lost productivity, wages, etc, for the patient on the day of the procedure), result in a substantial societal and healthcare system burden financially when endoscopy is used in this setting as a routine diagnostic test.
Thus, referring every patient with reflux symptoms for endoscopy is not justifiable, given the substantial cost coupled with the poor sensitivity…
It is my recommendation that referral for endoscopy in a patient with suspected GERD should be reserved for patients with symptoms of GERD who also have alarm symptoms (discussed below), those patients who do not respond to a trial of empirical therapy with a PPI, or those in whom the diagnosis of GERD remains uncertain after initial assessment. Additionally, endoscopy may also have value in the patient with well-established and well-controlled GERD symptoms as a screening exam for Barrett’s esophagus (a premalignant condition in which the normal squamous epithelium of the esophagus is replaced in varying degree by a metaplastic specialized columnar epithelium).[3]”