“Exposure of the heart to ionizing radiation during radiotherapy for breast cancer increases the subsequent rate of ischemic heart disease”
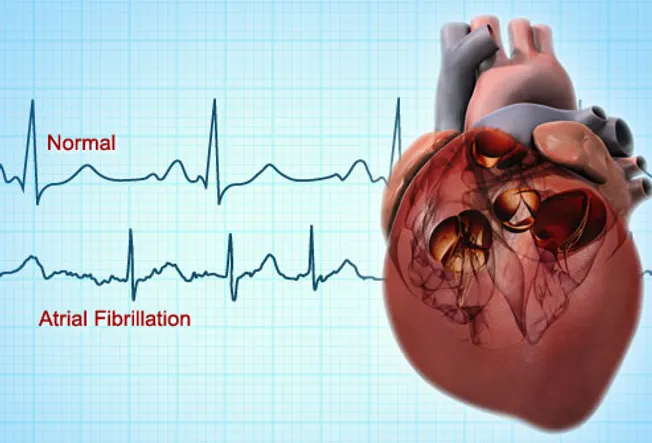
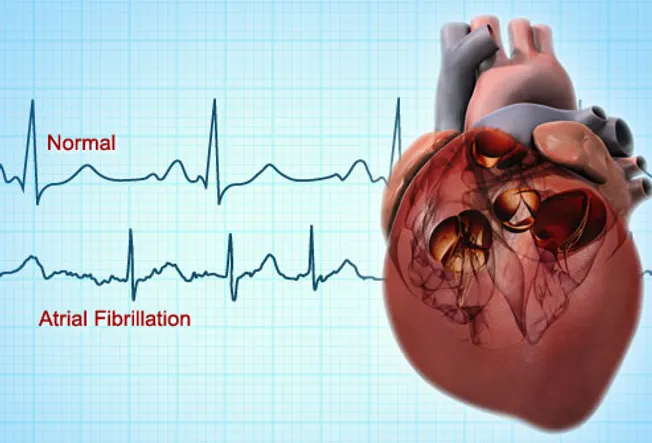
My mom and I both live with atrial fibrillation. My a-fib is chronic aka 24/7 and mom’s a-fib comes and goes. Both of our heart damage came as side-effects from cancer therapy.
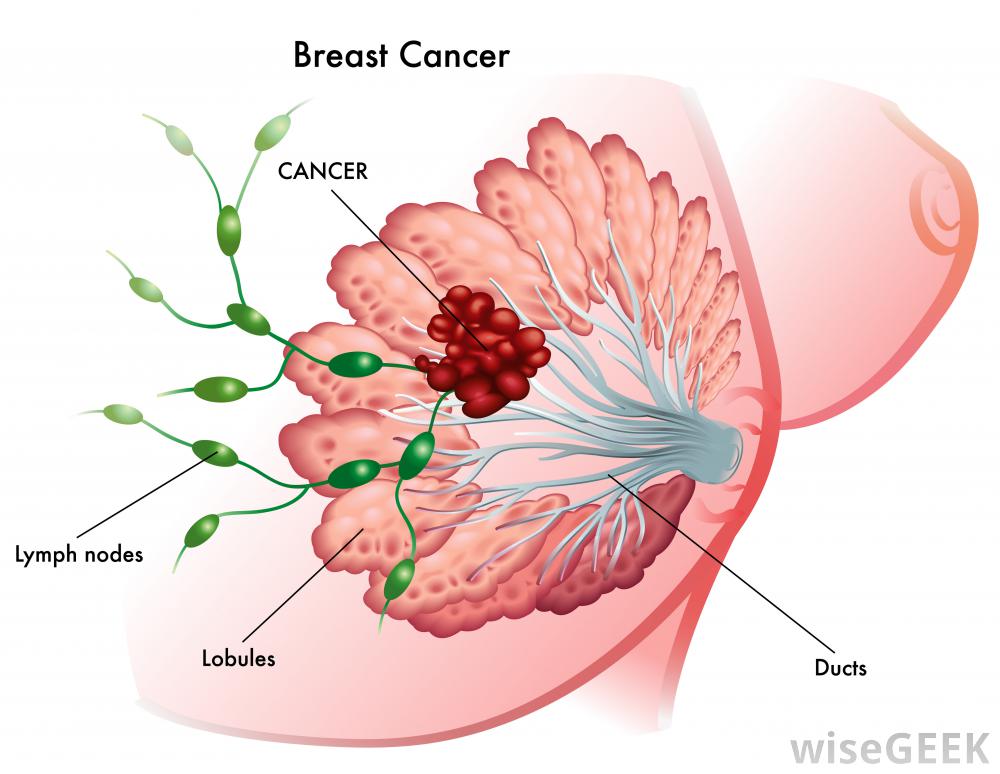
I was diagnosed with a blood cancer called multiple myeloma in early 1994. Mom was diagnosed with DCIS (BC stage 0) at the age of 75.
My heart disease came as late stage side-effect caused by cardio-toxic chemotherapy (adriamycin, melphalan, busulphan, cytoxan) and mom’s heart disease was caused by radiation from early breast cancer.
Two very different types of cancer. Two very different people. Two completely different oncologic therapies. Same long-term side effect.
The study linked and excerpted below says that the if you undergo radiation as a breast cancer therapy there is a real risk of heart damage. The more radiation you undergo, the greater the risk. The heart damage may show up after only a few years after radiation therapy (long-term) or 20 years after radiation therapy (late stage).
The point of this post is to draw attention to the damage to the human heart when a person undergoes either chemotherapy and or radiation. Further, as the research below indicates, this collateral damage can be reduced or eliminated.
Yes, I pursue several of these therapies. But no, I haven’t completely healed my chemo-induced heart damage yet. I did manage to stop the worsening of my heart damage in 2016, according to diagnostic testing such as regular echo cardiograms.
For more information about evidence-based, non-conventional therapies to prevent or reduce the risk of chemo and radiation-induced heart damage scroll down the page, post a question and I will reply ASAP.
Thank you,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
“Six studies were included in the review, including three randomized clinical trials and three nonrandomized clinical trials. Patients in five of six studies received anthracyclines. The results suggested that CoQ10 provides some protection against cardiotoxicity or liver toxicity during cancer treatment…”
“Radiation therapy has value in breast cancer, but the benefit comes at the price of an increased risk of ischemic heart disease later, researchers reported.
In a population-based case control study, the risk of major coronary events rose after radiation therapy by a mean of 7.4% for every gray (Gy) of exposure to the heart, with no apparent threshold, according to Sarah Darby, PhD, of the Clinical Trial Service Unit in Oxford, England, and colleagues.
The increase in risk was greatest in the first 5 years after radiotherapy but persisted for at least 2 decades, Darby and colleagues reported in the March 14 issue of the New England Journal of Medicine.
In addition, women with preexisting cardiac risk factors had greater absolute increases in risk, the researchers reported.
“Clinicians may wish to consider cardiac dose and cardiac risk factors as well as tumor control when making decisions about the use of radiotherapy for breast cancer,” Darby and colleagues concluded.
The study – among 2,168 breast cancer survivors in Sweden and Denmark — is a wake-up call for physicians, commented Jean-Bernard Durand, MD, of the MD Anderson Cancer Center in Houston.
“We have to be extra vigilant with women, making sure we assess them. We make sure they’re on correct medicines and we make sure they gain all of the benefits from surviving breast cancer,” he told MedPage Today.
Durand noted that in the U.S., women are much less likely than men to receive preventive cardiovascular care; changing that would help to mitigate the risk highlighted by Darby and colleagues.
“Follow their cholesterol, watch for diabetes, manage their blood pressure – all those things can be done to lower their risk of a cardiovascular event,” he said.
The study also highlights the importance of good post-cancer follow-up, he said.
Doctors “have an opportunity to intervene in a young woman and really change the course of her life rather than wait for an event and try to change the course of her life when she’s older,” Durand said.
Radiotherapy for early-stage breast cancer has been shown to reduce both recurrence and death, the researchers noted, but the effect of incidental exposure to the heart has not been clear.
They looked at women with breast cancer who had radiotherapy between 1958 and 2001, including 963 women with major coronary events and 1,205 controls.
Case patients had no recurrence of the breast cancer or incidence of any other cancer before they suffered a major coronary event, defined as myocardial infarction, coronary revascularization, or death from ischemic heart disease.
Controls were matched for country of residence, age at diagnosis, and year of diagnosis, and also had not had a recurrence of their breast cancer or any new malignancy.
Of the major coronary events among women in the study, 44% occurred less than 10 years after the breast cancer diagnosis, 33% occurred in the next decade, and the remaining 23% occurred still later.
The average dose to the heart was 6.6 Gy for women with left breast tumors, 2.9 Gy for those with cancer in the right breast, and 4.9 Gy overall.
While the rate of events rose by 7.4% per Gy of exposure, the rate varied with time — 16.3% in the first 5 years after exposure, 15.5% in the second 5 years, 1.2% in the second decade, and 8.2% in later years.
The only tumor characteristic that significantly affected the risk was location, as women with left breast tumors were more significantly likely to be case patients (P<0.001).
The rate ratio for women who had a history of ischemic heart disease, compared with those who did not, was 6.67 (95% CI from 4.37 to 10.18). Rate ratios were also elevated for women with other circulatory diseases, diabetes, or chronic obstructive pulmonary disease, as well as smokers.
The researchers cautioned that few of the women in the study were under 40, so the results may not apply directly to that age group.
In an accompanying editorial in the journal, Javid Moslehi, MD, of Brigham and Women’s Hospital in Boston commented that the findings may be the “tip of the iceberg.”
“In addition to ischemic cardiac disease,” he wrote, “radiation therapy has been associated with other cardiac conditions, including pericardial disease, peripheral vascular disease, cardiomyopathy, valvular dysfunction, and arrhythmias.
Those diseases were not part of the study, nor were those associated with some forms of chemotherapy, he noted.
One implication for practice, he argued, is that the time to look at cardiovascular issues is at the time of breast cancer diagnosis and before treatment starts.”
“Background:Radiotherapy for breast cancer often involves some incidental exposure of the heart to ionizing radiation. The effect of this exposure on the subsequent risk of ischemic heart disease is uncertain…
Rates of major coronary events increased linearly with the mean dose to the heart by 7.4% per gray (95% confidence interval, 2.9 to 14.5; P<0.001), with no apparent threshold. The increase started within the first 5 years after radiotherapy and continued into the third decade after radiotherapy. The proportional increase in the rate of major coronary events per gray was similar in women with and women without cardiac risk factors at the time of radiotherapy.
CONCLUSIONS: Exposure of the heart to ionizing radiation during radiotherapy for breast cancer increases the subsequent rate of ischemic heart disease. The increase is proportional to the mean dose to the heart, begins within a few years after exposure, and continues for at least 20 years. Women with preexisting cardiac risk factors have greater absolute increases in risk from radiotherapy than other women. (Funded by Cancer Research UK and others.).