Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Home-Based Cardiac Rehab- Underused
Home-Based Cardiac Rehab- Underused

Cardiac Rehabilitation (CR) programs reduce morbidity and mortality rates in adults with ischemic heart disease, heart failure, or cardiac surgery but are significantly underused, with only a minority of eligible patients participating in CR in the United States.
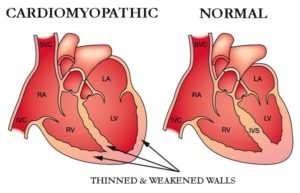
Mine is a fairly typical heart failure (HF) story. Chemotherapy-induced Atrial fibrillation (Afib) diagnosed in late 2010. The medical report from that appoitment also referred to dialated cardiomyopathy (DCM) but I wasn’t paying attention.
I am a long-term cancer survivor and I was focusing on all things cancer at the time.
Which, in some ways, may have helped my dialated cardiomyopathy. DCM was formally diagnosed in early 2019.
My dialated cardiomyopathy worsen only a bit between my afib diagnosis in lat 2010 and my formal CM diagnosis in early 2019 because my diet was clean, little alcohol, frequent exercise and nutritional supplementation that was pretty heart healthy. My ejection fraction (EJ) remained 40-45, my valves all appear to function well, and my blood pressure and weight are all normal for my age.
My point is that I was living the life of a cancer survivor which, as it turns out, was similar to what I now understand is a sort-of “home-based cardiac-rehabilitation” (HBCR) program. Let me give you some examples that are both anti-cancer as well as heart healthy.
- Whole-body hyperthermia (sauna)
- Curcumin supplementation
- Grapeseed Extract supplementation
- Omega-3 fatty acid supplementation
- CoQ10 supplementation
- Frequent, moderate exercise
- Diet full of fruits, veggies, whole grains-
- Moderate alcohol (red wine 2-3 x weekly)
Those are the therapies I pursued as a long-term cancer survivor. I got serious about managing my DCM when I was formally diagnosed on 2/1/19. I’ve since added heart healthy therapies or formalized the therapies above. Formalizing my sauna, for example, means that I take a 15 minute sauna daily instead of a longer sauna once or twice a week.
I was reading a post to a Facebook forum for cardiomyopathy survivors last week. The poster said that they didn’t “qualify” for cardiac rehabilitation coverage. I took that to mean that her health insurance would not pay for her to go someplace to recieve formal cardiac rehabilitation instruction.
What am I missing. All of the therapies listed above are supported by research. Should I be doing more? Less? I do my version of home-based cardiac rehabilitation.
Why do DCM survivors need to go somewhere to practice this therapy?
Scroll down the page, post a question or a comment and I will reply to you ASAP.
Thanks.
David Emerson
- Cancer Survivor
- Cancer Coach
- Director The Galen Foundation
Recommended Reading:
- Heart Failure-Cardiac Rehabilitation & Exercise
- Whole-Body Hyperthermia aka Sauna for Heart Disease
- Exercise vs. Drugs to Lower Blood Pressure?
Home-Based Cardiac Rehabilitation: A Scientific Statement From the AACPR, the AHA, and the ACC.
“Cardiac rehabilitation (CR) is an evidence-based intervention that uses patient education, health behavior modification, and exercise training to improve secondary prevention outcomes in patients with cardiovascular disease.
CR programs reduce morbidity and mortality rates in adults with ischemic heart disease, heart failure, or cardiac surgery but are significantly underused, with only a minority of eligible patients participating in CR in the United States.
New delivery strategies are urgently needed to improve participation.
One potential strategy is home-based CR (HBCR). In contrast to center-based CR services, which are provided in a medically supervised facility, HBCR relies on remote coaching with indirect exercise supervision and is provided mostly or entirely outside of the traditional center-based setting.
Although HBCR has been successfully deployed in the United Kingdom, Canada, and other countries, most US healthcare organizations have little to no experience with such programs.
The purpose of this scientific statement is to identify the core components, efficacy, strengths, limitations, evidence gaps, and research necessary to guide the future delivery of HBCR in the United States. Previous randomized trials have generated low- to moderate-strength evidence that HBCR and center-based CR can achieve similar improvements in 3- to 12-month clinical outcomes.
Although HBCR appears to hold promise in expanding the use of CR to eligible patients, additional research and demonstration projects are needed to clarify, strengthen, and extend the HBCR evidence base for key subgroups, including older adults, women, underrepresented minority groups, and other higher-risk and understudied groups. In the interim, we conclude that HBCR may be a reasonable option for selected clinically stable low- to moderate-risk patients who are eligible for CR but cannot attend a traditional center-based CR program.