Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
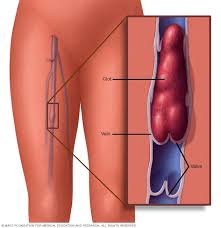
- Hospitalized? Reduce Blood Clot (VTE) Risk-
Hospitalized? Reduce Blood Clot (VTE) Risk-
Patients with an acute medical illness such as pneumonia, stroke, or congestive heart failure are highly susceptible to the development of venous thromboembolism (VTE) during their hospital stay and up to 3-months postdischarge.1,2
When I read the study linked below I remembered that my wife’s grandmother died because of a blood clot while in a hospital. Grandma wasn’t in the hospital because of heart failure or a stroke. She had broken her leg. Nothing major, just a broken leg…
I developed venous thromboembolism (VTE), a blood clot, days after I began chemotherapy. Both my cancer, multiple myeloma, and my chemotherapy regimen increase the risk of VTE. I wish I had read the article linked and excerpted below before I began my chemo.
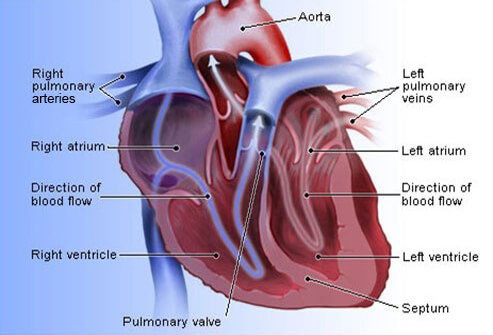
VTEs have been an ongoing feature of my health ever since my diagnosis of cancer back in 1994. I developed atrial fibrillation in late 2010. The main challenge you face when your heart beats irregularly is that blood can pool in a corner of your heart causing your blood to clot.
Of course if that clot happens to travel outside of your heart it can lodge in one of the tiny blood vessels (capillaries) in your brain. This blockage can cause a clot (stroke) and stop blood from getting to an area of your brain. This is bad…
I tried supplementing with warfarin about 20 years ago and couldn’t handle the side effects and long term risk of bleeding. So I did some research and now supplement with a number of evidence-based, non-toxic supplements that function as my own version of thromboprophylaxis.
My point is that VTE’s, blood clots, are common side effects of many facets of hospitalizations. Do yourself a favor and prepare for the possibilitiy of a VTE.
- Learn more about chemotherapy-induced cardiomyopathy- click now
- Learn More About Blood Clots aka Deep Vein Thromboses- click now
If you’d like to learn more about evidence-based but non-toxic therapies to reduce your risk of VTE, scroll down the page, post a question or comment and I will reply to you ASAP.
thank you,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
Proportion of US Hospitalized Medically Ill Patients Who May Qualify for Extended Thromboprophylaxis
“Extended thromboprophylaxis with oral anticoagulation can reduce the risk of symptomatic venous thromboembolism (VTE) in high-risk patients.
We sought to estimate the proportion of medically ill patients in the United States who might qualify for extended thromboprophylaxis according to the criteria used in the Medically-Ill Patient Assessment of Rivaroxaban versus Placebo in Reducing Post-Discharge Venous ThromboEmbolism Risk (MARINER) trial.
We analyzed 2014 National Inpatient Sample (NIS) data that provide a 20% weighted annual sample of all discharges from US acute-care hospitals.
Hospitalizations for acute medically ill patients were identified as those with a primary discharge diagnosis code for:
- heart or respiratory failure,
- ischemic stroke,
- infection, or
- inflammatory diseases.
Patients were excluded if they were <40 years old, admitted for surgery or trauma, had a length of stay <3- or >35-days, or were contraindicated to nonvitamin K antagonist oral anticoagulants. The modified International Medical Prevention Registry on Venous Thromboembolism (IMPROVE)-VTE score was used to stratify patients’ risk for postdischarge VTE, with a score of 2 to 3 suggesting patients were at moderate- and ≥4 as high-risk.
Of the 35 358 810 hospitalizations in the 2014 NIS, 1 849 535 were medically ill patients admitted for
- heart failure (10.1%),
- respiratory failure (12.2%),
- ischemic stroke (8.8%),
- infection (58.5%), or
- inflammatory diseases (10.4%).
The modified IMPROVE-VTE score classified 1 186 475 (64.1%) of these hospitalizations as occurring in moderate-risk and 407 095 (22.0%) in high-risk patients. This real-world study suggests a substantial proportion of acute medically ill patients might benefit from extended thromboprophylaxis using the modified IMPROVE-VTE score and clinical elements of the MARINER trial...
Patients with an acute medical illness such as pneumonia, stroke, or congestive heart failure are highly susceptible to the development of venous thromboembolism (VTE) during their hospital stay and up to 3-months postdischarge.1,2
Randomized controlled trials (RCTs).3–6suggest that high-risk medically ill patients can reduce their risk of symptomatic VTE by initiating thromboprophylaxis in-hospital and continuing extended thromboprophylaxis for up to 6 weeks postdischarge but at the potential cost of additional bleeding.7 ..
Conclusion: