
Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- How to juggle Hypercalcemia, Kidney Damage & Multiple Myeloma!!!
How to juggle Hypercalcemia, Kidney Damage & Multiple Myeloma!!!
“…said their data contradicts the notion that bone lesions are the primary cause of hypercalcemia (HC), noting that 91.2% of patients in their study had bone destruction, but only 16.8% had hypercalcemia.”
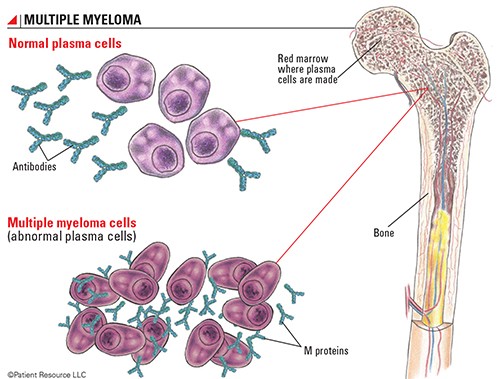
The study linked and excerpted at the bottom of the page below sparked an “AHA!” moment for me. I have always read that Multiple Myeloma causes bone destruction- which caused hypercalcemia. If you read the top study linked below, this thinking was common and contradicts the bottom study below.
According to bottom study below, 91% of MM patients present at diagnosis with bone destruction yet only 16.8% present with Hypercalcemia.
Long-story short, the study raises more issues than it addresses. Like many aspects of MM, oncology does not understand how/why a person with MM can experience bone destruction yet NOT have Hypercalcemia.
What then, does the newly diagnosed MM patient do about this symptom at diagnosis or at any point during his/her life as a MM patient?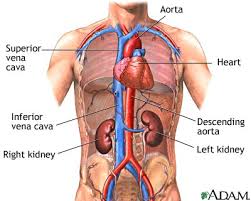
- According to research, Bisphosponate therapy is the first choice for MM patients who are dealing with Hypercalcemia.
- Be aware however, that Bisphosponates can cause kidney damage.
- If your MM has also damaged your kidneys and you want to manage Hypercalcemia, consider Xgeva. According to studies, this therapy can control Hypercalcemia without causing kidney damage.
- Side note: Xgeva is expensive. Make sure your health insurance will pay for it.
Both Bisphosponate therapy and Xgeva come with possible side effects. Osteonecrosis of the Jaw (ONJ) in particular. Like many therapies for health problems caused by MM, various therapies are a trade-off between risks and benefits.
If you are struggling with newly diagnosed MM and Hypercalcemia and kidney involvement you may be a bit overwhelmed. Please email me with questions, comments, etc.
and hang in there.
Thanks,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Muscles Help Long-term Multiple Myeloma Survival
- Multiple Myeloma X-ray, Diagnostic Testing Explained
- Chemo-Brain- Almost Half of Myeloma Patients
Multiple myeloma/hypercalcemia
“Hypercalcemia in myeloma
In myeloma patients, the primary cause of the hypercalcemia is widespread tumor-induced bone destruction…”
Treatment of hypercalcemia
“Severe hypercalcemia — Patients with As described immediately above, patients with an acute rise in serum calcium to more moderate levels who have changes in sensorium (eg, lethargy, stupor) also require aggressive therapy…
The concurrent administration of zoledronic acid (ZA; 4 mg intravenously [IV] over 15 minutes) or pamidronate (60 to 90 mg over two hours). ZA is preferable because it is superior to pamidronate in reversing hypercalcemia related to malignancy. (See ‘Bisphosphonates’ below and ‘Dosing in renal impairment’ below.)
●For patients with hypercalcemia in whom bisphosphonates are contraindicated (eg, due to severe renal impairment), denosumab can be administered concurrently with calcitonin. (See ‘Denosumab’ below.)
●Avoidance of calcium-containing foods and supplements and vitamin D…”
Hypercalcemia in Multiple Myeloma Leads to Poor Prognosis
New research attempts to answer some of the mystery related to the causes and impact of hypercalcemia in patients with newly diagnosed multiple myeloma.
Hypercalcemia is caused by many factors in patients with newly diagnosed multiple myeloma (NDMM) and is associated with poor rates of survival, according to a new study.
Hypercalcemia of malignancy (HCM) is a metabolic complication of cancer that occurs when humoral mechanisms like parathyroid hormone related protein- (PTHrP) or 1,25-dihydroxy vitamin D-mediated pathways and direct bone metastasis…
Hypercalcemia can occur in various types of malignancies, but the highest rates have been reported in MM.
In such cases, local osteolytic bone lesions are thought to be the primary cause, the investigators wrote…
Bao and colleagues said there is little existing research into key questions about hypercalcemia in MM, such as the proportion of hypercalcemia caused by humoral hypercalcemia of malignancy (HHM) or local osteolysis, and the association between hypercalcemia and bone metabolism in patients with MM.
The researchers set out to change that by evaluating the prognostic impact and mechanism of hypercalcemia in patients with symptomatic NDMM. Their findings were published in the journal Cancer Medicine…
Of the 357 patients, 16.8% had HC at the time of diagnosis, and those patients had some common laboratory results.
“The presence of HC was associated with higher serum levels of
- β2 microglobulin,
- creatinine,
- phosphorus,
- uric acid,
- procollagen I N‐terminal peptide,
- β‐carboxy‐terminal cross‐linking telopeptide of type I collagen and osteocalcin,
- lower serum levels of hemoglobin,
- parathyroid hormone (PTH),”
the authors wrote, adding that these patients also had higher stages on the MM International Staging System (ISS) and revised ISS (R-ISS).
Of all of those factors, the authors said serum PTH, hemoglobin, creatinine, and uric acid levels were the primary factors affecting HC.
Patients who had HC faced significantly worse survival rates, with a median of 40 months compared to 57 months in patients without the complication. The negative prognostic effect held up both in a univariate analysis and in a multivariate model that included adjustments for age and R-ISS stage.
Bao and colleagues said their data contradicts the notion that bone lesions are the primary cause of HC, noting that 91.2% of patients in their study had bone destruction, but only 16.8% had HC.
“Thus, HC mainly caused by localized bone disease could not well explain our clinical insights,” the investigators said. While local bone lesions seem to be related to HC, they said, such lesions are not the most important factor.
Instead, the authors suspect that humoral HC is the main cause of HC in MM. They said the high rate of kidney impairment (81.8%) among patients with severe HC suggests the kidneys have an important role in HC. They said anemia appears to be indirectly related with HC.
Still, the authors said many questions remain, and the findings of this study will need to be replicated, given the limits of a retrospective study.
Reference
Bao L, Wang Y, Lu M, et al. Hypercalcemia caused by humoral effects and bone damage indicate poor outcomes in newly diagnosed multiple myeloma patients. Cancer Med. Published online November 4, 2020. doi:10.1002/cam4.3594

