Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
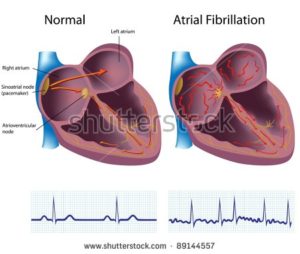
- Myeloma- Sudden Cardiac Death – Afib
Myeloma- Sudden Cardiac Death – Afib

“…calls for the need to “examine treatment modalities in addition to anticoagulation” to reduce sudden cardiac death (SCD) rates in patients with atrial fibrillation.”
I have chronic atrial fibrillation aka Afib. If you’re reading this blog post, you probably have Afib too.
I am a survivor of a blood cancer called multiple myeloma. But I’m thinking that the issue here is Afib and sudden cardiac death.
When I read the article below, I couldn’t help but wonder if I/we have a real risk of sudden death.
I wondered if I might drop dead at any moment. Or what my risk of this happening might be. And then how I might reduce that risk…
Let’s break it down.
Of the group of patients examined- Afib patients who died over a bit less than a 3 year period, “1,668 (71%) died from cardiovascular reasons.” It makes sense to me that our hearts are problematic and not as healthy as they would be otherwise. I don’t know about your Afib but mine was a caused by cardiotoxic chemotherapy. But that’s another blog post.
But I spend a fair amount of time and effort keeping my heart as healthy as I can.
Of those Afib patients who died for cardiovascular reasons, almost 45% of those died of sudden cardiac death aka SCD. These SC deaths accounted for almost a third of those who died for cardiovascular reasons. So of us Afib patients who die from a malfunctioning heart, almost half of us die from SCD. That seems like a large percentage to me.
What do you think?
The study gets sort of fuzzy from there. The closest the study comes to nailing down cause and effect between Afib and SCD is to say that “amongst the predictors (of SCD) they found
- older age,
- ejection fraction <50%,
- New York Heart Association functional class III‒IV and
- prior myocardial infarction.”
As a person living with cardiomyopathy, my take on that statement is that the people who die of SCD have a sicker heart on average than other heart failure patients. No magic here, just statistical analysis of a group of afib patients who die for cardiovascular reasons who have weak hearts.
The bottom line, as I see it, is that yes, Afib patients have an increased risk of sudden cardiac death. But the degree or size of this risk is largely based on how sick your heart it. Yes, Afib means your heart is sick. But it could be worse.
- I’m in my early sixties
- My EJ is 55%
- I believe my NYHA class is II
- and I have never had a heart attack
Ed. Note- five echocardiograms from the years 2015-2021 indicate stable or improving heart health- I have summarized the findings below.
- To Learn More about Chemotherapy-induced Heart Damage- click now
- To Learn More about chemotherapy-induced atrial fibrillation- click now
Do you have a weak heart?
Thanks
David Emerson
- Myeloma Survivor
- Myeloma Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Catheter Ablation no better than Drugs for AFib
- Living With Chronic Atrial Fibrillation with Non-Conventional Therapy
- Xarelto Lawsuit Highlights Risks of Conventional Blood Thinners
- Coffee, Afib, Cardiomyopathy and Cancer Survivor
Sudden cardiac death is the most common cause of death in atrial fibrillation patients, ENGAGE AF-TIMI 48 shows
“An analysis from the ENGAGE AF-TIMI 48 trial has found that SCD was the single most common cause of death and accounted for about a third of all deaths and nearly half of all cardiovascular deaths amongst 2,349 atrial fibrillation patients.
The report, published in the current issue of the Journal of the American Heart Association by Alon Eisen (Brigham and Women’s Hospital, Boston, USA and Harvard Medical School, Boston, USA) and others, calls for the need to “examine treatment modalities in addition to anticoagulation” to reduce SCD rates in patients with atrial fibrillation.
Recent data suggest that atrial fibrillation is independently associated with an increased risk of sudden cardiac death. “In patients with established atrial fibrillation treated with anticoagulation, SCD accounts for >20% of all deaths. In addition, patients with atrial fibrillation have, on average, a 2.5-fold increased risk of SCD or ventricular fibrillation compared with patients without atrial fibrillation,” write Eisen et al.
The authors note that there is not complete clarity on the mechanism underlying the causal association between SCD and atrial fibrillation. “Although atrial fibrillation and SCD share common risk factors such as heart failure or coronary artery disease, the association between atrial fibrillation and SCD does not seem to be entirely dependent on these risk factors,” the authors comment. Therefore, they set out to examine the incidence, characteristics, and factors associated with sudden cardiac death in a contemporary large cohort of patients with atrial fibrillation…
From 2,349 patients who died over a median follow-up of 2.8 years, 1,668 (71%) died from cardiovascular reasons. Eisen et al found that sudden cardiac death was the single most common cause of cardiovascular death with 749 patients, accounting for 31.7% of all deaths and for 44.9% of all cardiovascular deaths. Heart failure or shock, fatal ischaemic stroke and fatal bleeding were other common causes of cardiovascular death with 390 (23.4%), 146 (8.8%) and 124 (7.4%) deaths respectively.
The authors also highlight that patients who experienced SCD were mostly men (70.6%) with a median age of 73 years. The majority had persistent or permanent atrial fibrillation (82.9%), had heart failure symptoms at baseline (72.9%) a CHA2DS2-VASc score of ≥4 (75.4), and a lower ejection fraction.
In order to identify independent predictors of SCD, the researchers used a multivariate competing risks analysis using the sub-distribution hazard model accounting for other cardiovascular death and for non-cardiovascular death. Amongst the predictors they found older age, ejection fraction <50%, New York Heart Association functional class III‒IV and prior myocardial infarction.
Male sex, electrocardiographic left ventricular hypertrophy, higher heart rate, non-use of beta blockers, and use of digitalis were found as additional significant baseline predictors of SCD, but not of other causes of death. Particularly, Eisen et al highlight that digitalis, was associated with sudden cardiac death regardless of heart failure status, which adds to the “concern” regarding digitalis treatment in patients with atrial fibrillation with or without heart failure…”
Echocardiogram Results from 2015-2021
- BP.
- left ventricle systolic function EF
- left atrium
- right atrium
- Aortic root-
- Ascending Aorta
All have improved or remained stable-
- 6/2021 BP- 109 /65 mmHg
- 2/2020 BP –109 /65 mmHg
- 10/2018- BP -126 /82 mmHg
- 9/2016- BP –125 /80 mmHg
- 10/2015-BP –114 /69 mmHg
6/2021 Left Ventricle: The left ventricular systolic function is low normal, with an estimated ejection fraction of 50-55%.
2/2020- Left Ventricle: The left ventricular systolic function is low normal, with an estimated ejection fraction of 50-55%.
10/2018- Left Ventricle: The left ventricular systolic function is mildly decreased, ejection fraction of 40-45%.
9/2016- Left Ventricle: The left ventricular systolic function is mildly to moderately decreased, with an estimated ejection fraction of 40-45%.
10/2015-The left ventricular systolic function is mildly decreased, with an estimated ejection fraction of 40-45%.
- 6/2021 Left Atrium: The left atrium is normal in size.
- 6/2021 Right atrium is upper limits of normal in size
- 2/2020- Left Atrium: The left atrium is severely dilated.
- 2/2020- Right Atrium: The right atrium is moderately dilated.
- 10/2018- Left Atrium: The left atrium is severely dilated.
- 10/2018- Right Atrium: The right atrium is mildly dilated
- 9/2016- Left Atrium: The left atrium is moderate to severely dilated.
- 9/2016 – Right Atrium: The right atrium is mildly dilated
- 10/2015- Left Atrium: The left atrium is mildly dilated
- 10/2015 – The right atrium is normal in size.
- 6/2021- Ao Root d: 5.10 cm
- 6/2021- Asc Ao, d: 4.60 cm
——–
- 2/2020- Ao Root-?
- 2/2020-Asc Ao, d: 4.60 cm
——–
- 10/2018- Ao Root: 4.40 cm
- 10/2018-Asc Ao, d: 4.60 cm
——–
- 09/2016- Ao Root- 4.3 cm
- 09/2016 – Asc Ao- 4.9 cm
——————
- 10/2015- Ao Root: 5.30 cm
- 10/2015– Asc Ao- 4.80 cm
2/2020 The aortic root is abnormal. There is moderate dilatation of the ascending aorta. There is severe dilatation of the aortic root.
10/2018- The aortic root is abnormal. There is moderate dilatation of the ascending aorta. There is moderate dilatation the aortic root.
09/2016- The aortic root is abnormal. There is moderate dilatation of the ascending aorta. There is severe dilatation of the aortic root.
10/2015- The aortic root is abnormal. There is moderate dilatation of the ascending aorta. There is severe dilatation of the aortic root. Maximal diameter of aortic root is 5.3 cm