
Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Kyprolis Inc. Survival, Dec. Quality of Life- Myeloma
Kyprolis Inc. Survival, Dec. Quality of Life- Myeloma
Multiple Myeloma patients assigned to the carfilzomib-containing regimen had a median overall survival (OS) of 48.3 months versus 40.4 months for patients who received lenalidomide and dexamethasone
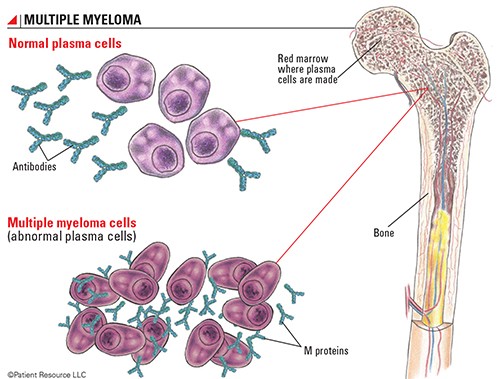
Multiple myeloma is incurable but very treatable. The study linked below is an excellent example of this confusing statement. Adding a chemotherapy called carfilzomib (Kyprolis) to Revlimid and dex chemo cocktail will, on average, increase a relapsed/refractory MMer’s response and potentially help the MMer live an average of eight (8) months longer.
Chemotherapy causes collateral damage aka side effects. Everyone knows this. One of the goals of PeopleBeatingCancer.org is to educate cancer patients, survivors, and caregivers about the pros and cons of conventional therapies.
Longer OS is a pro, serious side effects are a con.
The price to be paid for that eight months of life is a significant increase in the seven (7) side effects listed below. So yes, MM is incurable but yes, chemo cocktails continue to increase remissions.
Your challenge is that you may experience multiple side-effects during those eight months.
If you have any questions please scroll down the page, post a question or comment and I will reply to you ASAP.
Thank you,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Multiple Myeloma- Carfilzomib Cardiotoxicity, MRD Neg, DKRd Clinical Trial
- Multiple Myeloma Symptoms Cloud Multiple Myeloma Side Effects-
- Myeloma Therapy- Conventional, Complementary, Integrative –
New Analysis Confirms Carfilzomib Survival Benefit in Relapsed/Refractory Myeloma
“The addition of carfilzomib (Kyprolis) to lenalidomide (Revlimid) and dexamethasone for relapsed/refractory multiple myeloma led to a statistically significant 21% reduction in the risk for death compared with lenalidomide and dexamethasone…
Patients assigned to the carfilzomib-containing regimen had a median overall survival (OS) of 48.3 months versus 40.4 months for patients who received lenalidomide and dexamethasone…
“The addition of carfilzomib resulted in a higher objective response rate, a tripling of the complete response rate, significant and clinically relevant prolongation of both progression-free and overall survival…
Adverse event (AE) rates were similar between the treatment groups including all-grade AEs (98.0% in both groups),
- grade ≥3 AEs (87.0% with carfilzomib vs 83.0% for the control group),
- serious adverse events (65.6% vs 56.8%),
- discontinuation due to AEs (33.4% vs 30.1%), and
- grade 5 AEs (11.5% vs 10.5%).
Updated safety data showed that all-grade nonhematologic events were generally more common in the experimental arm for
- diarrhea (44.4% vs 37.3%),
- fatigue (33.4% vs 31.9%),
- cough (29.6% vs 18.0%),
- pyrexia (fever) (29.8% vs 21.6%),
- upper respiratory infections (30.1% vs 20.8%),
- hypokalemia (29.6% vs 14.9%), and
- muscle spasms (27.0% vs 21.1%).
With respect to grade ≥3 adverse events, only hypokalemia in the carfilzomib arm (10.5%) affected as many as 10% of patients in either group…
Also, while survival benefit was greater in the (kyprolis) higher dose group, patients and their physicians must also consider the possibility of increased side effects, such as peripheral neuropathy, before upping their dose.”
The challenge with multiple myeloma chemotherapy regimens is that they have dramatic pros and dramatic cons. MM chemotherapy can kill your MM while it kills your body.
For the record, when I say “increased side effects” I am talking about adverse events discussed in the articles linked below. I am talking about the general issue of quality of life vs. quantity of life. Further, increasing the dose of carfilzomib/kyprolis can increase the PFS experienced by both the newly diagnosed MMer as well as the relapsed MMer according to the studies below.
I’m not talking about those short-term side effects such as nausea, fatigue, losing your hair, etc. that we’ve all come to expect with chemo and radiation. Grade 3 or higher adverse events such as heart damage, nerve damage (CIPN), or severe AE’s causing discontinuation of therapy, etc. can have a dramatic impact on the life of a MMer.
If you or a loved one have been diagnosed with Multiple Myeloma, let me say this loud and clear:
It is critical that you become an active participant in your care. Learn everything you can.
I am alive today largely because I took the time to find out everything I could about Multiple Myeloma and sought out the full spectrum of evidence-based MM therapies both conventional (FDA approved) and non-conventional.
Please watch the video below to learn more about the evidence-based, integrative therapies to combat treatment side effects and enhance your chemotherapy.
Recommended Reading:
- Multiple Myeloma Patients are ALL “Toxicity-Vulnerable”
- Carf. Induced Heart Damage in Multiple Myeloma
- Multiple Myeloma- Newly Diagnosed Without Intent to ASCT
New Analysis Confirms Carfilzomib (kyprolis) Survival Benefit in Relapsed/Refractory Myeloma
“The addition of carfilzomib (Kyprolis) to lenalidomide (Revlimid) and dexamethasone for relapsed/refractory multiple myeloma led to a statistically significant 21% reduction in the risk for death compared with lenalidomide and dexamethasone, according to a final analysis of the phase III ASPIRE trial...
- Adverse event (AE) rates were similar between the treatment groups including
- all-grade AEs (98.0% in both groups),
- grade ≥3 AEs (87.0% with carfilzomib vs 83.0% for the control group),
- serious adverse events (65.6% vs 56.8%),
- discontinuation due to AEs (33.4% vs 30.1%), and
- grade 5 AEs (11.5% vs 10.5%).”
Updated safety data showed that all-grade nonhematologic events were generally more common in the experimental arm for
- diarrhea (44.4% vs 37.3%), fatigue (33.4% vs 31.9%),
- cough (29.6% vs 18.0%),
- pyrexia (29.8% vs 21.6%),
- upper respiratory infections (30.1% vs 20.8%),
- hypokalemia (29.6% vs 14.9%), and
- muscle spasms (27.0% vs 21.1%).
With respect to grade ≥3 adverse events, only hypokalemia in the carfilzomib arm (10.5%) affected as many as 10% of patients in either group.”
Carfilzomib can lead to cardiovascular toxicity in multiple myeloma patients
“Researchers gathered data from 24 studies reported from 2007 through 2017, which included information on 2,594 MM patients. They found 18.1 percent of patients who took carfilzomib experienced CVAE, with 8.2 percent of those cases being grade three or higher, meaning they are categorized as severe. For comparison, a similar review of bortezomib, another proteasome inhibitor, found just 3.8 percent of patients experienced CVAE and only 2.3 percent were severe...
Increased Drug Dosage Could Improve Survival in Myeloma
“Patients with multiple myeloma could see additional survival benefit when adjusting their dosage of Kyprolis (carfilzomib) plus dexamethasone (a regimen referred to as “Kd”), according to recent research presented at the 2018 American Society of Hematology (ASH) Annual Meeting in San Diego.
“The objective of this research was to study the impact of carfilzomib, or Kd dosing in the real world, on two very important clinically relevant endpoints: overall survival and time to next treatment,” said study author Sumeet Panjabi, Ph.D., of Amgen.
The researchers examined the electronic medical records of more than 1,400 adults who were diagnosed with myeloma between January 2010 and October 2017; received a Kd regimen in any line of therapy; and had three or more doses of Kyprolis after their first administration of Kyprolis in the Kd regimen. Then, the cumulative weekly dose was calculated by the total of the weekly dose of Kyprolis divided by the number of weeks of the Kd treatment.
Two groups were prepared in the study – those who were given a cumulative weekly dose of 120 mg or more of Kd and those given less than 120 mg.
“So just recently in October, the (Food and Drug Administration; FDA) approved carfilzomib or Kd 70 mg weekly on the basis of the ARROW trial. The ARROW trial demonstrated the superiority of the 17 weekly Kd doses relative to the legacy dose, 27 mg per meters squared, twice weekly,” Panjabi said. “We call this the legacy dose because this was the first carfilzomib dose that had been approved way back in 2012. Also, in 2016, the FDA approved carfilzomib 56 mg per meters squared twice weekly on the basis of the ENDEAVOR trial, which demonstrated superiority of Kd over Velcade plus dexamethasone.”
Twelve-month overall survival for the higher dose group was significantly longer than in the lower dose group – 90.3 percent of patients versus 79.7 percent, respectively.
“Essentially, the takeaway here is that a higher treatment dose was associated with a higher probability of survival,” Panjabi said.
When it came to the time to the next treatment, the higher dose also bested the lower dose, with patients being able to wait longer periods between treatments. The average time to next treatment was 17.5 months in the higher dose group, and 13.2 months in the lower group. Further, about a third (32 percent) of patients given a higher dose experienced treatment progression after 12 months, compared to 44.8 percent in the lower dose group.
“This has the same takeaway as the survival results,” Panjabi said. “Higher treatment dose was associated with lower probability of progression to the next treatment.”
However, this study did have some limitations, warranting future investigation comparing the two dosing strategies. For example, the lower treatment dose group made up the majority of the sample (1,340 patients; 91.2 percent). This is because, as Panjabi mentioned, the higher dosage was not granted approval by the FDA until 2016, which was more than halfway through the study period.
Also, while survival benefit was greater in the higher dose group, patients and their physicians must also consider the possibility of increased side effects, such as peripheral neuropathy, before upping their dose.”



