“Patients who receive the standard surgical treatment for melanoma that has spread to one or more key lymph nodes do not live longer…
I understand how difficult it can be to make decisions about your therapy if you have been diagnosed with melanoma that has spread beyond the original site. You will be compelled to think about challenging issues such as your length of life and your quality of life.
Please understand that, “completion lymph-node dissection” dose not lead to longer life and may very will lead to lower quality of life according to the studies linked and excerpted below.
When I was originally diagnosed with my “incurable” cancer I did whatever my oncologist prescribed. Unfortunately every therapy Dr. Berger pushed led a possible increase of only months of life and lots of long-term and late stage side effects.
At the time of my conventional therapies (surgery, chemo and radiation) I didn’t know that there were many other evidence-based therapies that I could undergo that might improve my overall survival, as well as improve my quality-of-life.
It was a non-conventional therapy that put me into complete remission in 1999. Which is why I urge you to learn about evidence-based, non-conventional melanoma therapies. If your melanoma has spread beyond the original site, yes, you much seriously consider chemotherapy. But also consider evidence-based integrative therapies to enhance the efficacy of that chemotherapy in addition to evidence-based anti-melanoma, botanicals, nutrition, etc.
Have you been diagnosed with melanoma? What therapies are you considering? Please scroll down the page, post a question or comment and I will reply to you ASAP.
To Learn More About Melanoma- click now
Thank you,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
“There are numerous pros and cons of lymph node dissection for treating melanoma.
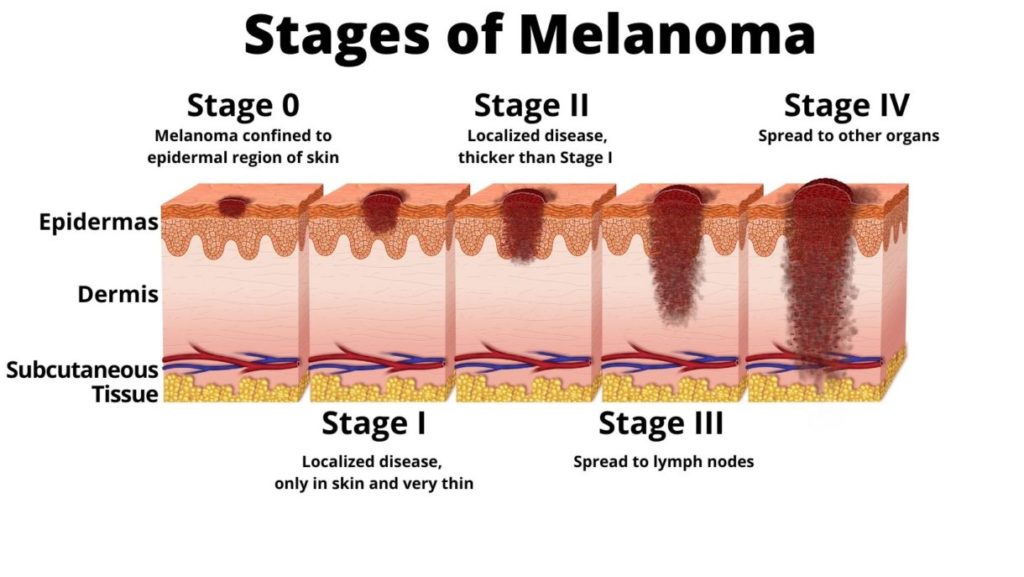
When melanoma is on the skin, it can be effectively and permanently removed in most cases. Sometimes, however, it spreads (metastasizes) to other areas of the body, usually traveling first to the nearest lymph nodesin your armpit, neck, or groin. If your healthcare provider suspects that this has happened, a test called a sentinel node biopsy will be performed to identify and remove the lymph node to which the cancer is likely to have spread from the primary tumor.1
If your sentinel node biopsy is positive (contains cancerous cells), then it’s decision time. Should you have all the other lymph nodes in this area removed, in a surgical procedure called completion lymph node dissection(CLND, or lymphadenectomy)? The idea is that a CLND ensures that the melanoma cells in all the other lymph nodes are removed, which then may prevent the disease from spreading farther.2…”
“Lymphadenectomy or lymph node dissection is the surgical removal of one or more groups of lymph nodes.[1] It is almost always performed as part of the surgical management of cancer. In a regional lymph node dissection, some of the lymph nodes in the tumorarea are removed; in a radical lymph node dissection, most or all of the lymph nodes in the tumor area are removed.[2][3][4]…
Indications[edit]
It is usually done because many types of cancer have a marked tendency to produce lymph node metastasis early in their natural history. This is particularly true of melanoma, head and neck cancer, differentiated thyroid cancer, breast cancer, lung cancer, gastric cancer and colorectal cancer. Famed British surgeon Berkeley Moynihan once remarked that “the surgery of cancer is not the surgery of organs; it is the surgery of the lymphatic system”.[citation needed]
The better-known examples of lymphadenectomy are axillary lymph node dissection for breast cancer; radical neck dissection for head and neck cancer and thyroid cancer; D2 lymphadenectomy for gastric cancer; and total mesorectal excision for rectal cancer.[citation needed]
BACKGROUND-Sentinel-lymph-node biopsy is associated with increased melanoma-specific survival (i.e., survival until death from melanoma) among patients with node-positive intermediate-thickness melanomas (1.2 to 3.5 mm). The value of completion lymph-node dissection for patients with sentinel-node metastases is not clear…
RESULTS- Immediate completion lymph-node dissection was not associated with increased melanoma-specific survival among 1934 patients with data that could be evaluated in an intention-to-treat analysis or among 1755 patients in the per-protocol analysis.
In the per-protocol analysis, the mean (±SE) 3-year rate of melanoma-specific survival was similar in the dissection group and the observation group (86±1.3% and 86±1.2%, respectively; P=0.42 by the log-rank test) at a median follow-up of 43 months. The rate of disease-free survival was slightly higher in the dissection group than in the observation group (68±1.7% and 63±1.7%, respectively; P=0.05 by the log-rank test) at 3 years, based on an increased rate of disease control in the regional nodes at 3 years (92±1.0% vs. 77±1.5%; P<0.001 by the log-rank test); these results must be interpreted with caution. Nonsentinel-node metastases, identified in 11.5% of the patients in the dissection group, were a strong, independent prognostic factor for recurrence (hazard ratio, 1.78; P=0.005). Lymphedema was observed in 24.1% of the patients in the dissection group and in 6.3% of those in the observation group.
CONCLUSIONS-Immediate completion lymph-node dissection increased the rate of regional disease control and provided prognostic information but did not increase melanoma-specific survival among patients with melanoma and sentinel-node metastases…”
“Patients who receive the standard surgical treatment for melanoma that has spread to one or more key lymph nodes do not live longer, a major new study shows…
The study, published today in The New England Journal of Medicine, found that immediately removing and performing biopsies on all lymph nodes located near the original tumor, a procedure called completion lymph node dissection, did not result in increased overall survival rates.
…the most important question facing physicians and those newly diagnosed with the disease: whether patients who have melanoma cells in a limited number of lymph nodes should undergo extensive surgery to remove all the remaining nodes in that area of the body. The results of the new research suggest they do not…
Additionally, nearly 25 percent of the patients who underwent the completion dissections suffered from lymphedema, compared with about 6 percent of the control group, the study found. Lymphedema is swelling that may result when lymph nodes are damaged or removed. Symptoms include hardening of the skin, infections and restricted range of motion.
“This is a larger operation that has a higher risk of complications,” Faries said, “including wound infection and nerve damage…”