
Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Lytic Lesions Increase Risk of Death in Multiple Myeloma
Lytic Lesions Increase Risk of Death in Multiple Myeloma
The research findings show the importance of preventing bone disease (lytic lesions) in multiple myeloma…”
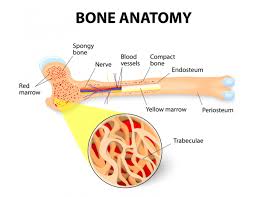
Lytic lesions and bone damage as a symptom of multiple myeloma before or after diagnosis is highlighted in the study linked and excerpted below. According to research, there are two main issues:
- Patients with MM and fractures are at a significantly increased risk of death
- Patients with MM and bone disease have a reduced quality of life,
It’s fine for a study to confirm a finding. Lytic lesions increase your risk of death. Fine. The real issue, in my opinion, is to provide information, actionable therapies, shown to heal bones, build bone strength, basically fix the problem highlighted by the study.
Let me also say that it is entirely possible that conventional, FDA approved therapies such as steroids such as dexamethasone, may be part of the reason for the study findings below. By this I mean that FDA approved bone therapies are limited and therefore may be part of the problem.
Standard-of-Care bone therapy in multiple myeloma:
- Bisphophonates-
- Denosumab-
- Kyphoplasty:
Evidence-based, non-conventional bone therapy in multiple myeloma:
- Nutrition-
- Supplementation-
- Complementary therapies-
As always, I find a study that is relevant to multiple myeloma survival and I am proposing a combination of conventional MM therapies as well as evidence-based non-conventional therapies. Lytic lesions for MM patients and survivors are a clear indication that MM is as much of a blood disease as it is a bone disease.
If you’ve developed lytic lesions or bone involvement along with your MM, the study linked below is your incentive to work to build bone health for the rest of your life.
Have you been diagnosed with MM? Are you experiencing lytic lesions aka bone damage? Scroll down the page, post a question or a comment and I will reply to you ASAP.
- To learn more about managing your bone health, click now
- Click now to learn more about death and the myeloma survivor
Hang in there,
David Emerson
- MM Survivor
- MM Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Cancer Prehabilitation-
- Bone Imaging Can Make or Break Multiple Myeloma
- End Stage Multiple Myeloma- Early Palliative Care
The Role of Bisphosphonates in Multiple Myeloma: Mechanisms, Side Effects, and the Future
“Despite rare toxicities noted with the long-term use of BPs and the development of new bone-targeted therapies, BPs remain an important part of cancer supportive therapy and the standard of care for MM bone disease. Regardless of the long history of BPs in the clinic, ongoing clinical trials are evaluating new doses and schedules of administration of both Pam and ZA in MM patients, alone and in combination with new bone therapies, investigating their role in the prevention of bone disease in early-stage MM, and prospectively assessing the frequency of some of the more recently observed side effects…”
Kyphoplasty for Patients With Multiple Myeloma is a Safe Surgical Procedure: Results From a Large Patient Cohort
“Introduction: Only in recent years has balloon kyphoplasty gained significance in the treatment of vertebral fractures as an adequate minimally invasive vertebral stabilization technique. Kyphoplasty has also increasingly been used to treat vertebral osteolyses caused by multiple myeloma (MM)…
Results: Painful osteolytic or fractured vertebrae or even imminent vertebral instability caused by osteolyses were seen as indications for kyphoplasty. One case of pulmonary embolism was observed because of cement leakage as the only postoperative complication.
Conclusion: By careful interdisciplinary indication setting and a standardized treatment model, kyphoplasty presents a very safe and effective procedure for the treatment of vertebral osteolyses and fractures caused by MM.
Denosumab for bone lesions in multiple myeloma – what is its value?
“There appears to be no benefit from using denosumab instead of zoledronic acid in terms of overall survival or skeletal events. In addition, the safety profile is very similar. There appears to be slightly more renal toxicity with zoledronic acid; however, this is balanced by the higher rates of hypocalcemia with denosumab.
Although there was a demonstration of benefit in terms of progression-free survival, this finding should be treated with caution, as it emerged from a post hoc exploratory analysis. There are, however, significant differences in costs – both to society and to patients. Denosumab costs approximately $24,000 more per patient per year in the USA…”
Fractures in Patients With MM Negatively Impact Survival, Study Says
“Due to the nature of the disease, multiple myeloma (MM) causes lytic bone lesions and fractures, but the impact of fractures on survival is unknown. A recent study indicates that patients with MM and fractures are at a significantly increased risk of death compared with patients who do not have fractures.
Patients with MM and bone disease have a reduced quality of life, as the interaction between malignant plasma cells in the bone marrow and the bone microenvironment leads to the destruction of bone and reduced osteoblast function, as well as blocking of bone repair. Fractures may be caused by decreased bone mineral density and treatment with glucocorticoids; in a previous population-based retrospective study, patients had a 9-fold increase in the risk of factors after MM diagnosis…
The adjusted results showed that patients with a fracture at diagnosis were at a significantly increased risk of death . The risk of death was significantly increased in patients with a fracture after MM diagnosis (HR, 2.00; 95% CI, 1.90-2.10).
The impact of fractures on survival did not change significantly between the 2 calendar periods—1990-1999 and 2000-2013—in the study (HR, 0.98; 95% CI, 0.89-1.08).
The authors said that patients with MM with fractures are at a significantly increased risk of dying compared with those without fractures. The findings show the importance of preventing bone disease in multiple myeloma, they said
Reference
Thorsteinsdottir S, Gislason G, Aspelund T, et al. Fractures and survival in multiple myeloma: results from a population-based study [published online December 2, 2019]. Haematol. doi:10.3324/haematol.2019.230011.


