Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- side effects ID and prevention »
- Mammography Under 40 Does More Harm Than Good?
Mammography Under 40 Does More Harm Than Good?
“young women have received screening mammography, but few cancers have been detected, regardless of their specific age, race, or other individual characteristics.”
The challenge of the studies below is the need of reading them carefully. Mammography can be a useful diagnostic test. But testing all women under 40, for example, causes more harm than good according to the bottom study.
If you are a young woman with no family history of breast cancer then you probably will not benefit from mammography. If however, your risk is above average then, according to the study, you may learn more from a diagnostic testing method other than mammography- an MRI or ultrasound.
I am a long-term survivor of a very different sort of cancer. I have learned that there are dozens of evidence-based non-toxic therapies that can reduce the risk of breast cancer or the risk of a breast cancer relapse.
For more information scroll down the page, post a question or comment and I will reply to you ASAP.
Thank you,
David Emerson
- Cancer Survivor
- Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Why a Cancer Coach?
- Chemo Brain Therapies in Breast Cancer
- Health Report: Breast Cancer and Chemicals
Benefits and Risks of Mammography Screening in Women Ages 40 to 49 Years
“Breast cancer screening in the United States is complicated by conflicting recommendations from professional and governmental organizations. The benefits and risks of breast cancer screening differ though by age which should influence shared decision-making discussions.
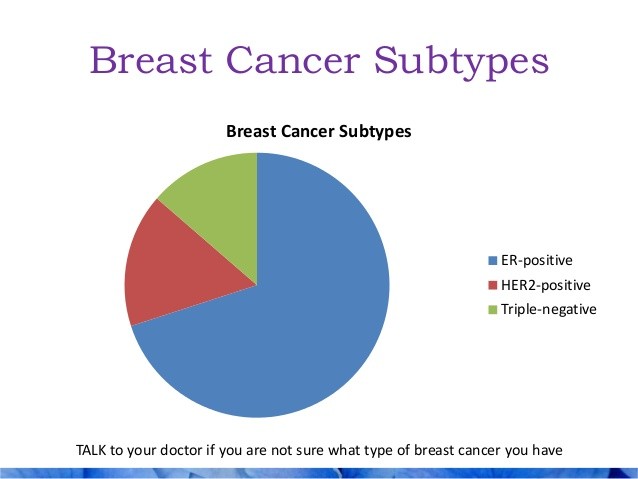
Compared to older women, women ages 40 to 49 years have a lower risk of breast cancer, but the types of breast cancer that develop are often more aggressive with a poorer prognosis.
Furthermore, younger women have a longer life expectancy and fewer comorbidities. The primary benefits of screening for women in their 40s are a reduction in breast cancer mortality, years of life lost to breast cancer, and morbidity of breast cancer treatment by detecting cancers at an earlier stage.
Compared to older women, the risks of breast cancer screening in women ages 40 to 49 years includes more false positive recalls and biopsies as well as transient anxiety.
Concerns regarding radiation induced malignancy and overdiagnosis are minimal in this age group. The shorter lead time of breast cancer in women ages 40 to 49 years also favors shorter screening intervals.
This information should help inform providers in their shared decision-making discussions with patients…”
Performance of First Mammography Examination in Women Younger Than 40 Years
Background Few data have been published on mammography performance in women who are younger than 40 years.
Methods We pooled data from six mammography registries across the United States from the Breast Cancer Surveillance Consortium. We included 117 738 women who were aged 18–39 years when they had their first screening or diagnostic mammogram during 1995–2005 and followed them for 1 year to determine the accuracy of mammography assessment. We measured the recall rate for screening examinations and the sensitivity, specificity, positive predictive value, and cancer detection rate for all mammograms.
Results For screening mammograms, no cancers were detected in 637 mammograms for women aged 18–24 years. For women aged 35–39 years who had the largest number of screening mammograms (n = 73 335) in this study,
- the recall rate was 12.7% (95% confidence interval [CI] = 12.4% to 12.9%), sensitivity was 76.1% (95% CI = 69.2% to 82.6%), specificity was 87.5%,
- the positive predictive value was 1.3%, and
- cancer detection rate was 1.6 cancers per 1000 mammograms.
Most (67 468 [77.7%]) of the 86 871 women screened reported no family history of breast cancer. For diagnostic mammograms, the age-adjusted rates across all age groups were: sensitivity of 85.7% (95% CI = 82.7% to 88.7%), specificity of 88.8% (95% CI = 88.4% to 89.1%), positive predictive value of 14.6% (95% CI = 13.3% to 15.8%), and cancer detection rate of 14.3 cancers per 1000 mammograms (95% CI = 13.0 to 15.7 cancers per 1000 mammograms). Mammography performance, except for specificity, improved in the presence of a breast lump.
Conclusions Younger women have very low breast cancer rates but after mammography experience high recall rates, high rates of additional imaging, and low cancer detection rates. We found no cancers in women younger than 25 years and poor performance for the large group of women aged 35–39 years. In a theoretical population of 10 000 women aged 35–39 years, 1266 women who are screened will receive further workup, with 16 cancers detected and 1250 women receiving a false-positive result.
Cancer Detection Rate per 1000 Mammograms. The overall age-adjusted cancer detection rate was 1.7 cancers per 1000 mammograms (95% CI = 1.4 to 1.9 cancers per 1000 mammograms). The cancer detection rate essentially did not change with age and was not associated with family history, particularly in the age group of 35–39 years (Table 2). African American women had higher cancer detection rates than white women. The cancer detection rate was higher among women with a lump (11.4 cancers per 1000 mammograms, 95% CI = 7.8 to 15.4) than among women without a lump (1.2 cancers per 1000 mammograms, 95% CI = 1.0 to 1.4) (P < .001).
Diagnostic Performance
In conclusion, young women have received screening mammography, but few cancers have been detected, regardless of their specific age, race, or other individual characteristics. With high recall and low cancer detection rates, many young women, who are at low or average risk for breast cancer, are having additional imaging as a result of undergoing screening mammography, with a low probability of cancer detection.
Who should be screened for breast cancer at younger ages and how best to screen them remain important research questions. Cancers in young women, across the board, have characteristics associated with more rapid tumor growth and poorer prognosis than those in older women.
Tumor characteristics with poorer prognostic characteristics pose a dilemma: It is important to find breast cancers in young women early because of the underlying tumor biology of such cancers; yet current screening performance is challenged by the high breast density, which is generally found in young women. Research results evaluating the performance of the addition of ultrasound and/or breast magnetic resonance imaging in young women at high risk for breast cancer are needed to show whether these modalities perform better than mammography alone in young women.