70-80% of multiple myeloma patients will have bone involvement, with risk for skeletal-related events…Bone lesions most commonly involve the vertebra, ribs, skull, pelvic bones and femur in descending order.
Multiple Myeloma is about more than a long list of facts and statistics. I get that. However, MM stats are a great way to bone up on the what, when and why of your rare, incurable blood cancer.
In the article below, I have highlighted the areas that discuss bone lesions: their causes and common treatment options. For the record, I don’t agree with some of what Dr. Cohen has listed below.
For example, my own bone damage healed. I have imaging film to see that the bone filled in. As rare cancer found primarily in people over 65, MM is not fully studied and not well-understood.
Overall, I think it’s important for Myeloma patients and survivors to think about how to manage Myeloma in terms of two goals:
- Alleviating and managing symptoms
- Stalling progression of the disease
Bone health is a huge component of both of these goals.
I am both a MM survivor and MM Cancer Coach. Living with MM since early ’94 has meant that I have had to take responsibility for my own health.
For example, bisphosphonate therapy for bone density is pretty much a standard addition to all newly diagnosed MMers’ therapies. After my own bisphosphonate therapy, I researched and learned about evidence-based, but non-FDA bone health therapies that incorporate nutrition, supplementation, and lifestyle therapies. I put all of this information into an easy-to-read guide for Myeloma survivors and caregivers to use.
To learn more about the other myeloma therapies and issues that I relied on to manage my own cancer since ’94, please click the blue button below to watch a FREE webinar, The Top Myeloma Issues and the Evidence-Based Therapies That Can Help.
To Learn More about Myeloma and Bone Involvement- click now
Let me know if you have any questions by commenting at the bottom of the page, and I will get back to you ASAP.
Thank you,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
“Dr. Stephen Cohen- Have you ever wanted to read the notes and observations of a practicing compassionate and empathetic doctor who has cared for cancer patients for over 40 years? Wel, now you can! Dr. Stephen Cohen, a medical oncologist and hematologist practicing in San Antonio, Texas, has kept a daily journal of interesting medical info and tidbits he encounters day to day from his personal experiences with patient care, professional journals he reads, and medically relevant information on all subjects that he comes across.’
- Estimated 30,000 new cases diagnosed in 2016, and an estimated 12,650 deaths.
- Myeloma represents 1.8% of all new cancer cases.
- Ranks as the 15th most common type of cancer in the United States.
- Increasing numbers of patients with MM due to an aging population.
- Ranks as the 15th most common type of cancer in the United States.
- Estimated that approximately 96,000 patients are living with multiple myeloma.
- Accounts for 1% of new cancers.
- Accounts or 2% of all cancer deaths in the U.S.
- Median age at diagnosis 65-70 years.
- The median age at death is 75 years, with mortality rate increasing as age increases.
- Fewer than 4% of patients younger than 45 years.
- Survival varies depending upon a host of factors: the stage of disease, biology including cytogenetic abnormalities and response to therapy.
- Disease biology is reflected in the molecular subtype of myeloma and the presence or absence of secondary cytogenetic abnormalities.
- A five-year survival rate of greater than 70% is present in transplant-eligible patients, 50% in the elderly transplant ineligible patients.
- Chromosome abnormalities detected with cytogenetics or fluorescence in situ hybridization in more than 90% of cases and include deletions, trisomies, and translocations.
- In a study using CT scans to assess patients with multiple myeloma and undergoing bisphosphonate therapy found in annual fracture incidence of 14%, all of which were vertebral compression fractures (Vogel MN et al).
- Treatment is challenging due to the fact that patients are usually of advanced age, have disease-related factors including comorbidities conditions such as cardiac processes, renal impairment and have had cardiac events.
- The presence of asymptomatic lytic lesions implies a poor prognosis with the median time to progression for smoldering myeloma of less than one year, that explains why these lesions are excluded from patients with this diagnosis.
- At the time of diagnosis two-thirds of patients have bone pain and are likely to subsequently sustain pathological fractures, particularly of the skull, spine, and ribs.
- 70-80% of patients will have bone involvement, with risk for skeletal-related events.
- Extended survival associated with increased risk of skilled related events.
- Multiple myeloma bone lesions usually do not heal, and fractures can result in permanent disability and may require surgery or joint replacement.
- In patients with MM untreated for osteolytic lesions, the median time to first skeletal-related event is approximately 9 months (Berenson JR).
- The risk of fracture is higher than for cancer of the breast, prostate, or lung.
- Pathologic fractures associated with 20-44% increased the risk of death…
- At diagnosis, 5% have localized tumors, designated plasmacytomas, and 95% have systemic disease with bone marrow involvement.
- 80% of patients have osteolytic lesions.
- Most common symptoms on presentation are fatigue, bone pain and recurrent infections.
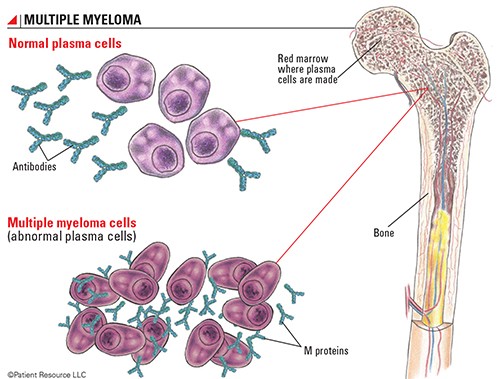
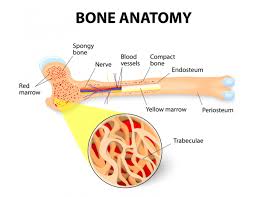
- Cortical bone and medullary compartments are linked anatomically but are functionally distinct.
- Bone findings result of either inhibition of osteoblastic activity and or activation of osteoclast activity.
- Cortical involvement results in endosteal scalloping, with an invasion of the periosteum and at times extraosseous extension.
- Bone lesions most commonly involve the vertebra, ribs, skull, pelvic bones and femur in descending order.
- Distal bone involvement is less common than proximal bone involvement.
- Diffuse osteopenia without focal bone lesions and sclerotic bone lesions may occur, uncommonly.
- Plasmacytomas mostly arise as the direct extension of skeletal tumors when they disrupt cortical bone.
- About 15% have hypercalcemia
- Conventional x-ray studies reveal skeletal abnormalities in approximately 80% of patients and include fractures, lytic lesions, and osteoporosis.
- Bone scans and serum alkaline phosphatase levels are normal due to the absence of osteoblast activity.
- The presence and extent of bone marrow and extramedullary involvement are important factors influencing prognosis and clinical management.
- Skeletal complications cause pain, disability, decreased mobility and impaired quality of life which can be improved with treatment.
- Surgery radiation therapy are used to treat pathological fractures and the use of bisphosphosphonates is the standard of care for preventing and reducing the rate of skeletal-related events in patients with bone metastases or osteolytic lesions.
- Bisphosphonates are activated in myeloma as they work by interrupting the recruitment, maturation, and attachment of osteoclasts.
- Bisphosphonates induce apoptosis in osteoclasts and in plasma cells.
- The imbalance between osteoclast activation and osteoblast suppression with suppression of bone formation leading to purely lytic lesions.
“The study was undertaken to determine how concurrent osteoporosis is associated with poorer outcomes in patients who develop MM, a blood cancer of aging adults. Primary osteoporosis is also highly prevalent in aging adults and is associated with increased mortality.
Of the 362 participants who developed incident MM, with an average 10.5 years of follow-up, 226 died, including 71 with high FRAX scores and 155 with low FRAX scores.
On average, women with high FRAX scores were 8.3 years older at enrollment (95% confidence interval [CI], 7.2-9.3 years) and 8 years older at time of MM diagnosis (95% CI, 7.0-9.2 years) compared with those with low FRAX scores.
MM mortality for women with high FRAX scores was greater (covariate-adjusted hazard ratio scores [aHR] 1.51; 95% CI, 1.01-2.25; P = .044) compared with those with low FRAX scores..”