Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Myeloma – Don’t Pay for Denosumab Unless…
Myeloma – Don’t Pay for Denosumab Unless…
“The study authors commented that routine use of denosumab in patients with multiple myeloma “is difficult to justify except in patients with renal dysfunction or in those unable to tolerate bisphosphonates”
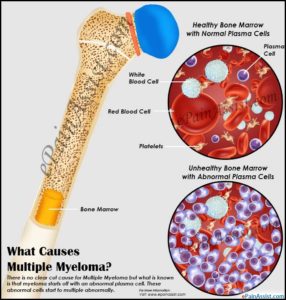
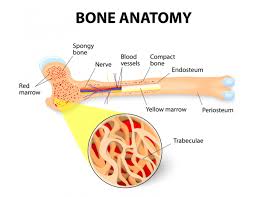
A diagnosis of multiple myeloma is life-changing. If you are like me you rely on your oncologist to recommend and prescribe those multiple myeloma chemotherapy regimens that are the “best” for you in every way. Consider zoledronic acid (bisphosphonates) vs. denosumab (xgeva).
When it comes to that MM chemotherapy that is meant to strengthen your bones, the concept of “best” is relative. I will tell you what surviving MM since early 1994 has taught me is “best” for newly diagnosed MM patients.
My experience is that you must walk the fine line between:
- efficacy and expense,
- cost and benefit.
According to both studies linked below, denosumab and zoledronic acid (bisphosphonates) are equally effective at:
- strengthening bones and
- side effects such as ONJ
The key reason in favor of denosumab is if you suffer from renal-impairment aka if your kidneys have been damaged by your MM. In other words, your oncologist will recommend Denosumab for you if your MM has damaged your kidney function.
The main challenge with denosumab
Densosumab is about nine times more expensive than zoledronic acid.
If you have a co-pay or deductible you have to learn about the dark side of MM chemotherapy regimens and how expensive they can be. And considering your oncologist may be paid a percentage of the cost of whatever multiple myeloma chemotherapy he/she prescribes, you have to wonder what the “best” mm chemotherapy is for you.
I am not saying that your oncologist has anything other than your best interests at heart. All I am saying is that you must be aware of the expense of your multiple myeloma chemotherapy and talk with your oncologist about what is best for you in your situation.
To Learn More about Bisphophonates- click now
To learn about the many evidence-based, non-toxic bone health therapies, scroll down the page, post a question or comment and I will reply to you ASAP.
Hang in there,
David Emerson
- MM Survivor
- MM Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Multiple Myeloma Chemotherapy = Accelerated Aging
- ‘Financial Conflict’ in Myeloma Oncologists’ Compensation?
- Multiple Myeloma Symptoms at Diagnosis- CRAB Explained-
Caution Urged When Considering Denosumab in Patients With Multiple Myeloma Who Have Normal Renal Function
“According to data published in a research letter in Lancet Oncology, the use of denosumab, a monoclonal antibody targeting receptor activator of nuclear factor-κB ligand (RANKL), for the prevention of skeletal-related events in older patients with multiple myeloma has increased dramatically, even in patients without renal dysfunction, following its January 5, 2018, approval by the US Food and Drug Administration (FDA) for this indication.1,2
The FDA approval of denosumab in the setting of multiple myeloma was based on results of a recent noninferiority trial that compared denosumab with the bisphosphonate zoledronic acid in patients with newly diagnosed multiple myeloma characterized by at least 1 lytic lesion and adequate renal function (ie, creatinine clearance of at least 30 mL/min) (NCT01345019). The findings from this study showed denosumab to be noninferior to zoledronic acid regarding time to skeletal-related events.3
Of note, while bisphosphonates, which are eliminated through the kidneys, are not recommended in patients with severe renal dysfunction given their association with renal toxicity,4 the pharmacokinetics and pharmacodynamics of denosumab are not affected by kidney function, although hypocalcemia has been reported in some patients with renal impairment receiving denosumab without adequate calcium supplementation.2
This retrospective analysis used Medicare fee-for-service claims data to investigate use of denosumab and bisphosphonates (eg, zoledronic acid, palmidronate) in older patients with multiple myeloma prior to (January 1, 2017, to January 4, 2018) and following (January 5, 2018, to March 31, 2019) FDA approval of denosumab in this setting.1
For the 15,872 patients included in the analysis, the percentage of denosumab used was only 0.1% of all bone-modifying doses used in the period prior to FDA approval, increasing to 38.1% in the post-FDA approval period.
Notably, large increases in denosumab uptake were noted in both patients with and without renal dysfunction, with adjusted incidence rate ratios of postapproval versus preapproval denosumab use of 17.9 and 36.0 in these 2 patient populations, respectively.1
Other characteristics of patients more likely to receive denosumab included older age and rural residence.1
The study authors commented that routine use of denosumab in patients with multiple myeloma “is difficult to justify except in patients with renal dysfunction or in those unable to tolerate bisphosphonates” given the increased expense and more frequent dosing of denosumab compared with bisphosphonate therapy, as well as the rapid bone loss associated with the discontinuation of denosumab.1
In their concluding remarks, the study authors stated that “further research should examine the role of rebates and reimbursements as incentives for the widespread adoption of more costly drugs that have not demonstrated superiority.”1
Disclosure: Some of the authors disclosed financial relationships with pharmaceutical and medical device companies. For a full list of disclosures, please refer to the original study.
Denosumab versus zoledronic acid in bone disease treatment of newly diagnosed multiple myeloma: an international, double-blind, double-dummy, randomised, controlled, phase 3 study
“This study aimed to assess the efficacy and safety of denosumab compared with zoledronic acid for the prevention of skeletal-related events in patients with newly diagnosed multiple myeloma…
The study met the primary endpoint; denosumab was non-inferior to zoledronic acid for time to first skeletal-related event…
Incidence of osteonecrosis of the jaw was not significantly different between the denosumab and zoledronic acid groups (35 [4%] vs 24 [3%]; p=0·147). The most common serious adverse event for both treatment groups was pneumonia (71 [8%] vs 69 [8%])…
In patients with newly diagnosed multiple myeloma, denosumab was non-inferior to zoledronic acid for time to skeletal-related events.”