Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Multiple Myeloma, Chronic Pain, Cure vs. Control
Multiple Myeloma, Chronic Pain, Cure vs. Control

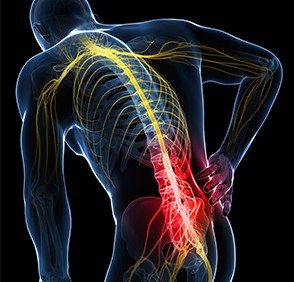
“Chronic pain is a major public health issue in the United States right now. And it’s the most common side effect of cancer (MM) treatment-Charles Jiang, MD,”
I’ll take the study linked below a step further and say that multiple myeloma (MM) survivors experience greater long-term pain, both from conventional MM therapies as well as from MM symptoms, than the average cancer survivor.
If, as Dr. Jiang says in the article below, chronic pain is the most common side effect of cancer treatment, then it stands to reason that the less treatment, the less chronic pain the patient experiences.
In the case of multiple myeloma, the cure versus control debate makes it clear that conventional MM oncology’s attempt to “cure” MM necessitates an aggressive or high-dose approach to treating MM.
Therefore, if conventional MM oncology follows the “cure” therapy approach when he/she treats the newly diagnosed MM, then the oncologist is condeming that MM patient to a lifetime of chronic pain.
Which describes my own multiple myeloma experience.
A misdiagnosis of pre-myeloma necessitated aggressive chemotherapy and radiation over a two year period. The aggressive chemotherapy and radiation resulted in a series of long-term and late stage side effects. These long-term and late stage side effects all cause chronic pain.
To add insult to injury, my conventional treatment resulted in two short remissions and two relapses and an end-stage diagnosis.
The point of this post is not for me to complain about conventional MM therapies. Multiple myeloma patients and survivors must utilize toxic therapies to control their cancer from time to time. The point of this post is to educate the MM patients about
- the importance of the cure vs. control debate in MM
- the importance of short, long-term and late stage side effets
- The importance of quality of life and quantity of life in MM
Conventional MM therapies can be effective. But only for a relatively short time. It is in the best interest of the multiple myeloma patient to think about all the issues that he/she faces.
To Learn More about Chemotherapy-induced Nerve Damage- click now
Have you been diagnosed with multiple myeloma? Scroll down the page, post a question or comment and I will reply to you ASAP.
thank you,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- A Long-term Multiple Myeloma Survivor’s Diet, Nutrition Plan-
- Chemotherapy, Heart Failure, and the Multiple Myeloma Survivor
- A Long-term Multiple Myeloma Survivor’s Diet, Nutrition Plan-
1 in 3 Survivors Still in Pain Years After Cancer Treatment
“Years after undergoing cancer treatment, about 1 in 3 cancer survivors — which represents about 5 million Americans — report that they are still in pain. Half of them say the pain is severe enough to limit their lives and their ability to work.
The finding comes from an analysis of data from 4526 people in the 2016–2017 National Health Interview Survey.
The study, published as a research letter in the June 20 issue of JAMA Oncology, once more highlights the dilemma faced by physicians obliged to provide effective pain relief in a world wracked by the opioid crisis.
“Chronic pain is a major public health issue in the United States right now. And it’s the most common side effect of cancer treatment,” said study lead Changchuan (Charles) Jiang, MD, of Mount Sinai Hospital in New York City.
“We are told to be cautious in giving the opioids because we don’t want to cause abuse, but there are concerned opinions from the oncologists, especially in palliative care, that sometimes we might be overcautious on giving opioids for the cancer patient,” he told Medscape Medical News.
Jiang suspected that chronic pain in cancer survivors was undertreated and underreported, but he was surprised by the scale of the problem uncovered by his team.
“I thought that chronic pain would be common in cancer survivors, but I never thought it would be this common,” he said. “It’s something that we’ve been highlighting [to medical colleagues], that pain management is the critical part of cancer survivorship care, but we still see so many patients suffering from chronic pain. That means we’re doing a poor job.”
Time Does Not Heal
Another finding that raised eyebrows was that time did not heal: more than 16 years after diagnosis, prevalence of chronic pain was holding steady at one third (34.8%) of cancer survivors, almost identical to the 36.4% prevalence seen within a year of diagnosis.
“It was a bit surprising to me that the prevalence of chronic pain did not change much with time from diagnosis,” said Jiang. “This needs to be highlighted — even if the patient has a remote cancer history, maybe 15, 20 years ago, they may still suffer from remarkable pain.”
The cause of chronic survivorship pain is often unclear. Nerve or tissue damage from surgery or radiation, small bone fractures, even undiagnosed metastases could be to blame.
Jiang and colleagues found that, among survivors younger than 65 years, people with private health insurance were one third (35.6%) less likely to experience chronic pain than were recipients of Medicaid, an income-based government benefit. (The age of 65 was the cutoff for this analysis because all Americans over 65 are eligible for Medicare.) In general, chronic pain was more prevalent among people with a less-than-high-school education, low household income, or no paid employment.
This study adds to the growing mountain of science documenting socioeconomic disparities in US cancer outcomes. “I was not really surprised that patients with low income had the most pain,” said Jiang. “We always see this socioeconomic disparity in everything in the healthcare service.”
One such example was the 2017 analysis of three US national databases showing that the poor are 22% more likely to die from their cancer than the wealthy.
Eliminating socioeconomic disparities in cancer in the US is a goal of the Centers for Disease Control’s Healthy People 2020 Initiative and the National Cancer Institute’s Center to Reduce Cancer Health Disparities (CRCHD).
Said Jiang, “One thing I can tell you for sure is that patients on Medicaid are doing very badly in terms of chronic cancer pain. This study can’t tell us why, but based on what we [already know] they may not have access to the pain management service.” Jiang blamed insurers who limit access to specialties such as palliative care or anesthesiology. Even when cancer survivors on Medicaid are prescribed effective medication, many can’t afford the co-pay, he said.
The fix won’t come easily.
Jiang calls for a “comprehensive effort from physicians, patient advocates, insurers and the healthcare system”.
Better Medicaid coverage for cancer pain management is not only best for patients but makes economic sense, he said. “We should pay attention to a patient’s pain. If these patients can’t work it’s a financial loss to the whole society and a severe burden to everyone.”
Healthcare practitioners should also do a better job of pain management. Clinical practice guidelines such as those from the American Society of Clinical Oncology is “progress,” Jiang said, but education is also needed, especially for primary care. These physicians are the front line for long-term cancer survivors yet are often ill prepared for the role. A study in 2015 found that only 14% of primary providers were “very confident” in their ability to address late-term physical adverse events in breast cancer survivors. (Cancer. 2015;121:1249-1256)
If Jiang could do just one thing to improve the situation? Educating primary care physicians, he said. “We are in the era of dramatic improvements in prognosis and we’re excited to see that. This means a growing cancer survivor community, and I don’t think the primary care doctor is getting enough training on how to take care of these patients. We need to do that job well.”