Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Multiple Myeloma Diagnosis w/ Heart, Lung, Kidney Disease- Poor Prognosis-
Multiple Myeloma Diagnosis w/ Heart, Lung, Kidney Disease- Poor Prognosis-

“Findings of this large analysis revealed the presence of a comorbidity at diagnosis in over 50% of multiple myeloma patients and also revealed that survival reduced with increasing numbers of comorbidities.”
What is the difference between a comorbidity in a newly diagnosed multiple myeloma (NDMM) patient and organ damage caused by the multiple myeloma in a NDMM patient? A comorbidity is a disease that exists in the newly diagnosed multiple myeloma (NDMM) patient before the diagnosis of MM and organ damage caused by the MM exists because of the MM itself.
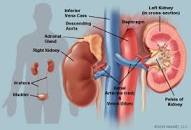
The first study linked below is about how comorbidities kill NDMM patients sooner than average and the study linked below that is about a common MM symptom- kidney damage. MM light chains (tiny proteins) can gum up a persons kidneys and damage the health of their kidneys. Kidney damage caused by your MM will kill you sooner than average the same way a comorbidity will.
In my mind, there is no difference to the patient. According to the studies linked below, both types of disease kill the patient sooner than MM alone. Depending on the seriousness of either/or/both, they can kill the patient A LOT sooner.
The difference, in my opinion anyway, is the treatment of disease whether you’re talking about treating:
- a comorbidity
- a symptom like renal damage
- or your MM itself.
The commonality between all three possible causes of death is treatment. The therapy (ies) that the patient undergoes in order to treat his/her comorbidity, his/her MM symptoms or the MM itself. Treatment is what keeps the NDMM patient alive.
In my blog post Multiple Myeloma Symptoms Cloud Multiple Myeloma Side Effects-
I made the argument that MM symptoms and the side effects caused by chemotherapy regimens for MM, from a length of life perspective, are the same. For example, it is virtually impossible for you or your oncologist to tell the difference between kidney damage caused by your MM or kidney damage caused by
- chemotherapy
- contrast imaging agents (gadolinium)
- NSAIDS (ibuprofen)
In this post, I am adding comorbidities to the mix. Many MM patients suffer from kidney damage as a comorbidity.
Study after study cite kidney involvement in MM yet the studies never document where the kidney injury occurred- as
- comorbidity
- as MM symptom or
- as MM side effect
Why should the NDMM patient care? The “standard-of-care” MM treatment plan is
- induction chemotherapy
- autologous stem cell transplant followed by
- maintenance chemotherapy
That is a LOT of chemotherapy. A LOT of toxicity for your body to handle. My personal and well as professional experience as a MM survivor and coach working with hundreds of MM patients is that whether comorbidity, symptom or side effect, less chemotherapy causes less damage.
To continue with the kidney example, there are a number of evidence-based but non-toxic supplements that both cause apoptosis to MM as well as protect or enhance kidney health. Curcumin and thymoquinone are two examples.
Have you or a loved one been diagnosed with MM? Are you suffering from comorbidities? Kidney damage? Scroll down the page, post a question or comment and I will reply to you ASAP.
Thank you,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
Multiple Myeloma Symptoms Cloud Multiple Myeloma Side Effects-
How to juggle Hypercalcemia, Kidney Damage & Multiple Myeloma!!!
Comorbidities in multiple myeloma and implications on survival: A population‐based study
“Researchers investigated the prevalence of comorbidities as well as their influence on survival in patients suffering from multiple myeloma.
This analysis involved 13,656 cases of multiple myeloma, with 7,404 (54%) having comorbidity at diagnosis. Elevated risk of death was found in patients suffering from one comorbidity at diagnosis vs those without any comorbidity, this risk was higher for patients with two and three or more comorbidities.
Patients with
- prior history of cancer,
- arrhythmia,
- heart failure,
- diabetes mellitus,
- cerebrovascular disease,
- chronic lung disease,
- psychological disease,
- peptic ulcer,
- neurological disease,
- peripheral vascular disease, c
- hronic kidney disease,
- dementia, and
- inflammatory bowel disease
were found to have increased risk of death. Findings of this large analysis revealed the presence of a comorbidity at diagnosis in over 50% of multiple myeloma patients and also revealed that survival reduced with increasing numbers of comorbidities. This highlights that comorbidities have importance when assessing patients and determining treatment approaches for patients with multiple myeloma.”
Defining Comorbidity: Implications for Understanding Health and Health Services
“Comorbidity is associated with worse health outcomes, more complex clinical management, and increased health care costs. There is no agreement, however, on the meaning of the term, and related constructs, such as multimorbidity, morbidity burden, and patient complexity, are not well conceptualized.
In this article, we review definitions of comorbidity and their relationship to related constructs. We show that the value of a given construct lies in its ability to explain a particular phenomenon of interest within the domains of
- clinical care,
- epidemiology, or
- health services planning and financing.
Mechanisms that may underlie the coexistence of 2 or more conditions in a patient (direct causation, associated risk factors, heterogeneity, independence) are examined, and the implications for clinical care considered.
We conclude that the more precise use of constructs, as proposed in this article, would lead to improved research into the phenomenon of ill health in clinical care, epidemiology, and health services…
DISCUSSION
Two main limitations of the present work need to be acknowledged. First, although the methods for searching the literature were valid, we cannot be certain that all relevant constructs and definitions have been identified. Second, our focus has been on professional concepts of comorbidity.
Although we have occasionally addressed the patient’s perspective, we have not consistently done so throughout the work. In particular, patients’ perspectives on the ways in which multiple conditions affect their health, well-being, and clinical care are highly relevant to the constructs of comorbidity considered here but have not been explicitly addressed.
We have defined the various constructs underpinning the co-occurrence of distinct diseases (comorbidity of an index disease, multimorbidity, morbidity burden, and patient complexity), described how these are interrelated, and shown how different constructs might best be applied to 3 different research areas (clinical care, epidemiology, health services)…”
Outcomes of newly diagnosed myeloma patients requiring dialysis: renal recovery, importance of rapid response and survival benefit
“About 50% of newly diagnosed multiple myeloma (MM) patients (NDMM) have some degree of renal impairment (RI) at presentation, up to 20% have severe acute kidney injury (AKI) and ~1–5% may require extrarenal dialysis, whereas severe RI is associated with high risk of early death and other complications.1, 2 Immediate effective anti-myeloma therapy and vigorous supportive care are the cornerstones of management.2, 3…