““All current FDA-approved MR contrast agents contain gadolinium, which in 2006 was associated with a devastating condition called nephrogenic systemic fibrosis in patients with impaired kidney function.”

Hi David – I have a fractured hip (pretty discouraging – my first fracture in 4 years). My MM oncologist wants to do an MRI. I asked for one without contrast based on the dangers of gadolinium, and he said “we don’t subscribe to that line of thinking.”
I’m not sure what that means – they don’t believe the studies, or they think the benefits of contrast outweigh the risks.
In any case, I said I would pass on the MRI. To your knowledge, are there any safe contrast agents out there?
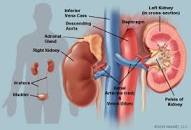
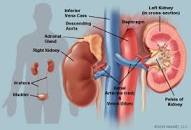
My most recent blood tests showed elevated creatinine, for the first time, so I’m very concerned about kidney health as well – another reason to avoid contrast.
Also, wanted to ask what you take for kidney health. I take Renafood by Standard Process – my naturopath thinks it’s a “wonder supplement”. But I want to be sure I have my bases covered.
Thank you!! Jane
Hi Jane-
I am sorry to read of your hip fracture. Ups and downs of the MM roller coaster. Hang in there.
Regarding your situation, I will reply to your questions below and then link studies that support my thinking at the bottom of the page.
First and foremost, you are correct. The standard-of-care, FDA approved, MRI contrast agent called gadolinium has been shown to:
- Spur/grow multiple myeloma
- build up, aka not leave the kidneys
- cause kidney damage
I will link studies below that confirm 1,2,3 above. This is not a “
line of thinking.” You are not advocating some sort of weird ideas. You are advocating
“evidence-based medicine.”The issue is not only that ONE MRI test is safe or that the benefits outweigh the risks for ONE MRI test. The issue that we MM survivors may have many MRIs over a period of years. According to research,
- gadolinium does build up in the kidneys and
- gadolinium can cause kidney damage and
- gadolinium does cause MM cells to grow.
Regarding your question “are their safe contrast agents-” Yes, there is a manganese-based contrast agent that, according to research, does not cause MM, and will be excreted from the body within 24 hours. I link the research below.
Regarding your question about supplements to manage or enhance kidney health, there are several supplements.
I don’t have experience with Standard Process’ supplement called
Renafood. However, I consider Standard Process to be the gold standard of nutritional supplementation.
According to research, these three supplements promote kidney health, prevent renal toxicity:
- Curcumin
- Resveratrol
- Vitamin D3
As you know, I am a huge fan of these three supplements for their anti-MM action as well as their bone health action.
All to say Jane, if you supplement with renafood, curcumin, resveratrol and vitamin D3 your kidney’s should be doing as well as can be expected…
Remember that other possible causes of kidney problems are:
Further, f you have light chains your MM may be clogging your kidney function. I forget your MM specifics. My point is that managing MM and managing our kidney health is an ongoing battle requiring an ongoing effort.
Let me know, thanks and kudos to you for standing your ground when talking to an oncologist who knows less than you do about MM.
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
“We observed that Omniscan induced both time and dose dependent MM cell growth in vitro (8-20 fold increase relative to control). Importantly, the presence of BMSC enhanced the effect of Omniscan on growth of both MM cell lines and primary MM cells..”
““All current FDA-approved MR contrast agents contain gadolinium, which in 2006 was associated with a devastating condition called nephrogenic systemic fibrosis in patients with impaired kidney function. We estimate that around 2 million contrast-enhanced scans are not performed in the U.S. every year because of the inability to use GBCAs in patients with poor renal function.”
“Gadolinium has been found to remain in patients’ bodies, including the brain, for months to years…1
The renoprotective effect of curcumin has been evaluated in several experimental models including diabetic nephropathy, chronic renal failure, ischemia and reperfusion and nephrotoxicity induced by compounds such as gentamicin, adriamycin, chloroquine, iron nitrilotriacetate, sodium fluoride, hexavalent chromium and cisplatin. It has been shown recently in a model of chronic renal failure that curcumin exerts a therapeutic effect; in fact it reverts not only systemic alterations but also glomerular hemodynamic changes. Another recent finding shows that the renoprotective effect of curcumin is associated to preservation of function and redox balance of mitochondria.
“Conclusions and Future Directions
Overall, all available in vitro and in vivo animal and human studies examining the effects of RSV in kidney disease indicate that it can reduce fibrosis, mesangial expansion, oxidative stress, and inflammatory cytokine levels, while improving kidney structure and function.
Treatment of renal mesangial, epithelial, and corpuscle cells with RSV resulted in reduced structural changes and ROS production, while antioxidant and mitochondrial activities were improved.
In addition, RSV treatment reduced fibroblast proliferation and activation to improve kidney structural maintenance. Renal cancer cells treated with RSV had reduced cell growth, cell-to-cell contact, and migration, and increased apoptosis…
The limited human studies indicate a protective effect of RSV administration on chronic kidney disease with increased kidney filtration rates and volume. The health benefits of RSV are widespread, and the low toxicity of the molecule makes it a prime candidate for medicinal use against kidney disease..”
“Recent observations have indicated that chronic kidney disease seems to be associated with a high incidence of nutritional vitamin D insufficiency or deficiency as manifested by decreased levels of 25-hydroxyvitamin D.
This contributes to the inability to maintain the levels of 1,25-dihydroxyvitamin D; therefore, current practice guidelines suggest repleting vitamin D status by the administration of native vitamin D as a first step in the therapy of the abnormalities of bone and mineral metabolism in chronic kidney disease.
The efficacy of this therapy is extremely variable, and active vitamin D sterols may be required, especially as kidney disease progresses…”