
Diagnosed with Cancer? Your two greatest challenges are understanding cancer and understanding possible side effects from chemo and radiation. Knowledge is Power!
Learn about conventional, complementary, and integrative therapies.
Dealing with treatment side effects? Learn about evidence-based therapies to alleviate your symptoms.
Click the orange button to the right to learn more.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Multiple Myeloma Prognosis- Cytogenetic Prognostic Index
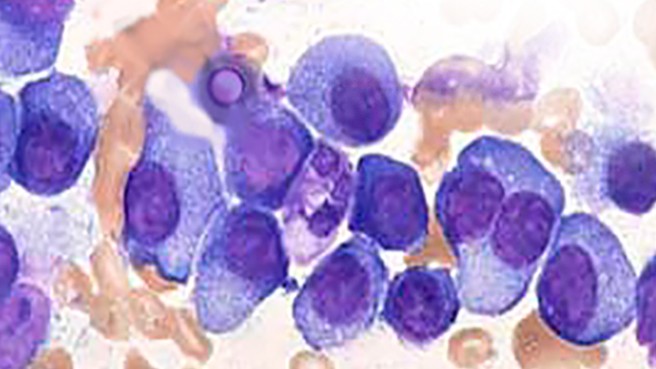
Multiple Myeloma Prognosis- Cytogenetic Prognostic Index
“The cytogenetic PI improves the classification of newly diagnosed patients with MM in the high-risk group compared with current classifications.”
A multiple myeloma prognosis of a newly diagnosed multiple myeloma (NDMM) patient is critical. While it is common to have your MM be genetically different from the average, differences can translate into poorer responses to chemotherapy regimens. And as we all know, “poorer responses” can mean shorter progression-free survival (PFS) and shorter overall survival (OR).
The challenge to the NDMM patient then, is how to identify and then treat cytogenetic abnormalities. The study linked and excerpted below explains how a MMer’s cytogenetic prognostic index supports the idea of identifying abonormalities.
When I sat down to write the post, my first thought was that I had no idea of what “normal” MM cytogenics are. I’ve been studying MM for years and I’ve never found a study talking about normal MM genetics- only studies citing ABNORMAL MM cytogenetics.
On the issue of what normal MM genetics are…is that MM is characterized by heterogeneity (diverse genetic make-up) so, as far as I can make out, abnormal cytogenetics is the presence of one of the differences. There is no “normal” only abnormal.
So if I understand the cytogenetic PI, it is a predictor of what happens if you, the NDMM, has one of the bad genetic abnormalities. And those are:
- del(17p);
- t(4;14);
- del(1p32);
- 1q21 gain; and
- trisomies 3, 5, and 21
If your genetic testing says that you have one or more of any of those markers, it means that your MM is more difficult to treat. More difficult to treat means shorter PFS and OS.
All the more reason to include a MM specialist on your team…
Have you been diagnosed with MM? Scroll down the page, post a question or comment to learn more about your increadibly complicated blood cancer.
Hang in there,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Your Diagnosis of Multiple Myeloma- A How-To Guide
- Bone Imaging Can Make or Break Multiple Myeloma
- Multiple Myeloma- How to Find and Work with the Best MM Specialists
Cytogenetic abnormality in patients with multiple myeloma analyzed by fluorescent in situ hybridization
“To analyze the fluorescent in situ hybridization (FISH) data and the association with clinical characteristics, therapy response, and survival time in patients with multiple myeloma…
Conclusion-
Multiple myeloma is characterized by a high occurrence of chromosomal aberrations. 1q21 amplification and t(4;14) are the most common abnormalities. Multiple cytogenetic abnormalities are frequently observed in the same one patient.
The total response rate, CR rate, and OS time are worse in cytogenetic abnormal patients compared with cytogenetic normal patients. Patients with 17p deletion have a very poor prognosis. Future goals of therapy will be to achieve minimal residual disease, biomarkers, and genomic data, which might provide a better estimate of the depth of response to therapy and OS…”
Development and Validation of a Cytogenetic Prognostic Index Predicting Survival in Multiple Myeloma
“The wide heterogeneity in multiple myeloma (MM) outcome is driven mainly by cytogenetic abnormalities. The current definition of high-risk profile is restrictive and oversimplified. To adapt MM treatment to risk, we need to better define a cytogenetic risk classification. To address this issue, we simultaneously examined the prognostic impact of del(17p); t(4;14); del(1p32); 1q21 gain; and trisomies 3, 5, and 21 in a cohort of newly diagnosed patients with MM.
Data were obtained from 1,635 patients enrolled in four trials implemented by the Intergroupe Francophone du Myélome. The oldest collection of data were used for model development and internal validation. For external validation, one of the two independent data sets was used to assess the performance of the model in patients treated with more current regimens. Six cytogenetic abnormalities were identified as clinically relevant, and a prognostic index (PI) that was based on the parameter estimates of the multivariable Cox model was computed for all patients.
In all data sets, a higher PI was consistently associated with a poor survival outcome. Dependent on the validation cohorts used, hazard ratios for patients in the high-risk category for death were between six and 15 times higher than those of patients in the low-risk category. Among patients with t(4;14) or del(17p), we observed a worse survival in those classified in the high-risk category than in those in the intermediate-risk category. The PI showed good performance for discriminating between patients who died and those who survived (Harrell’s concordance index greater than 70%).
The cytogenetic PI improves the classification of newly diagnosed patients with MM in the high-risk group compared with current classifications. These findings may facilitate the development of risk-adapted treatment strategies.”


