
Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Multiple Myeloma Prognosis- Stem Cell Transplant Post Induction or No?
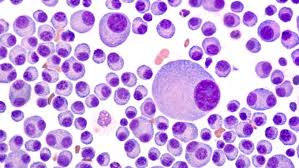
Multiple Myeloma Prognosis- Stem Cell Transplant Post Induction or No?
“The depth of response after induction and before ASCT determines patients’ prognoses after ASCT since the quality of response post induction and prior to ASCT are predictive of long-term PFS post ASCT13,33,44–49.”
Hi David- I am a newly diagnosed multiple myeloma (MM) patient (March 2019) undergoing treatment in Philly at Thomas Jefferson University Sidney Kimmel Cancer Center. I have an amazing medical team and I’m thankful for them everyday. When I was first diagnosed & admitted I was in really bad shape. I didn’t even know what MM was. I been undergoing weekly IV chemotherapy – Velcade and Cytoxan) since last March (with a 3-month break last summer).
My labs have been great all year since undergoing treatment. However, I am scheduled for an autologous stem cell transplant (ASCT) this May, 2020. I am very nervous.
I need to know what to expect from someone whose actually experienced it. Any insight you can provide would be great. Thank you in advance! Sally
Hi Sally,
I am sorry to read of your MM diagnosis. However, the Sidney Kimmel Cancer Center has a great reputation. Also, most of us have no idea what multiple myeloma is when we are first diagnosed.
My reply below is long. Please be sure to ask me any and all questions you may have.
If I understand your comments below, when you say that you were in “really bad shape” when you diagnosed and admitted, I take that to mean stage III, or advanced MM? Since then you have been undergoing induction therapy of Velcade, Cytoxan and dexamethasone or VCD or CVD?
When you say that your “labs have been great all year since undergoing treatment,” does that mean that you have reached MRD, complete remission, partial remission, etc? I am asking only because your response to induction therapy has a lot to do with your question about an autologous stem cell transplant.
Let me explain.
If you have been undergoing weekly, monthly chemotherapy since your diagnosis last March ’19 (with a 3 month break this past summer) your body has undergone, has had a lot of toxic therapy. Since you didn’t mention any side effects (nerve damage, blood clots, heart damage, chemobrain) I assume that you are managing all the toxicity pretty well.
However, studies continually show that the more toxicity a person undergoes, the higher the risk of short, long-term and late stage side effects. Your oncologist at Kimmel will confirm this.
Most all MM patients will assume this increased risk of side effects if it means that we will, on average, enjoy a longer PFS (progression-free survival is the first remission) or a longer OS (overall survival is total length of life).
When I talk about side effect in this case, I’m not only talking about nausea, losing your hair, etc. I’m talking about permanent peripheral neuropathy, heart damage, serious health issues like that. Health issues that can negatively affect a person’s quality of life.
My point is that we all balance risk with possible reward when we undergo toxic therapies.
In your case, the question is, will the risk of an ASCT immediately following your induction therapy be “worth it?” When you say “I need to know what to expect…” means what can happen to me that is bad, and what can happen to me that is good?
Bad and good aren’t very technical words but I’m trying to keep my explanation on a basic level here…
Studies show (many different studies) that, on average, if you have responded well to induction therapy (a good response if either MRD, CR or VGPR) then you will not achieve a longer OS (you won’t live longer) by having an ASCT. You may have a longer PFS (first remission).
However, the additional toxicity that results from an immediate ASCT, will risk short, long-term and late stage side effects.
All to say, you risk side effects and get little if anything, any benefits in return.
If you have not responded to your induction therapy with MRD, CR or VGPR, if your m-spike hasn’t been reduced much at all, then an immediate ASCT will, on average, increase your PFS and OS.
BTW, your oncologists should say the same thing I have above. Also, regardless of what you do, ASCT yes or no, harvesting your stem cells and storing them, is a good idea. A “just in case” sort of thing.
Let me know if you have any questions Sonya,
Hang in there,
David Emerson
- MM Survivor
- MM Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Stem Cell Transplant- Myeloma Secondary Cancer
- Multiple Myeloma Treatment Centers- “High-Volume Cancer Centers”
- Multiple Myeloma Response – MRD, sCR, CR, VGPR, PR ???
Current status of autologous stem cell transplantation for multiple myeloma
“…MRD negativity, defined as the absence of disease within one million bone marrow cells, has been examined due to its important prognostic value at different stages of the transplantation process.
The depth of response after induction and before ASCT determines patients’ prognoses after ASCT since the quality of response post induction and prior to ASCT are predictive of long-term PFS post ASCT13,33,44–49.
The final analysis of the IFM2009 prospective trial demonstrated the significance of MRD negativity, whereby patients achieving MRD negativity after induction with VRD had a similar OS irrespective of whether they received an ASCT or not50…”


