Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Chemo, Radiation-induced Muscle Atrophy
Chemo, Radiation-induced Muscle Atrophy

“Peripheral neuropathy can be part of a paraneoplastic syndrome accompanying the disease but more commonly is a consequence of treatment with neurotoxic therapies, and produces sensory, motor, autonomic nerve dysfunction or a combination.”
Multiple Myeloma side effects? All cancer patients expect chemo and radiation therapy to cause nausea, vomiting, our hair to fall out, etc. These are short-term side effects. But we don’t expect muscle atrophy.
I didn’t anyway. I walk with the help of hiking poles like the photo to the left.
The challenge with multiple myeloma side effects, in my experience anyway, is not the side effects themselves.
The problem is that not only did my oncologists NOT TELL ME about possible side effects, I don’t think Dr. Berger or Dr. Lazarus even knew that the chemo or the radiation they prescribed were going to cause the extensive damage that they caused! Certainly not extensive muscle atrophy.
Yes, dexamethasone is a chemotherapy drug. Research confirms that Dex. causes our muscle atrophy aka to shrink. In addition, the first article linked below is written by one of my oncologists, Dr. Hillard Lazarus. Dr. Lazarus documents the “sensory, motor, autonomic nerve dysfunction or a combination” caused by the chemotherapy and radiation that he and Dr. Berger prescribed for me.
Think about the ethics of my experiences as a multiple myeloma patient at University Hospitals. Did my oncologists prescribe therapies knowing the muscle atrophy and nerve damage that would result or did my doctors prescribe chemotherapy and radiation that they only suspected, might result in muscle and nerve damage?
Enough of my venting…
If you are a newly diagnosed multiple myeloma patient and you are about to undergo either/or/both chemo or radiation, can you reduce the risks extensive muscle atrophy and of other side effects? Yes. Keep in mind however, that the therapies that I am writing about are evidence-based but not approved by the FDA.
Resveratrol, HBOT, melatonin, exercise, others can all potentially reduce your risk of the multiple myeloma side effects that occurred to me.
- To Learn More about radiation dermatitis- click now
- To Learn More about therapy-related nerve damage- click now
- To Learn More about Palliative Cancer Care- click now
- To Learn More About Chemotherapy-induced nausea and vomiting- click now
To learn more, scroll down the page, post a question or comment and I will reply to you ASAP.
Hang in there,
David Emerson
- MM Survivor
- MM Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Multiple Myeloma Side Effects- Radiation-Induced Lumbosacral Plexopathy
- Multiple Myeloma Side Effects- Radiation Fibrosis Syndrome- Therapies
- Multiple Myeloma Side Effects- Heal Chemobrain, Prevent Dementia
Peripheral neuropathy in hematologic malignancies – Past, present and future
“Neurotoxic treatments (including proteasome inhibitors, immunomodulatory drugs and vinca-alkaloids) are often used in the treatment of hematologic malignancy. Peripheral neuropathy can be part of a paraneoplastic syndrome accompanying the disease but more commonly is a consequence of treatment with neurotoxic therapies, and produces sensory, motor, autonomic nerve dysfunction or a combination, leading to pain, loss of sensation and functional disability.
This review provides an update on peripheral neuropathy in hematologic malignancy, including risk factors, mechanisms and treatment options. We examine the clinical features and risk factors for peripheral neuropathy following bortezomib, thalidomide, brentuximab vedotin and vinca alkaloid treatment, as well as related compounds. We review the current data on pharmacogenetic risk factors for the development of toxicity and highlight areas of future research…”
RESVERATROL PREVENTS DEXAMETHASONE-INDUCED EXPRESSION OF THE MUSCLE ATROPHY-RELATED UBIQUITIN LIGASES ATROGIN-1 AND MURF1 IN CULTURED MYOTUBES THROUGH A SIRT1-DEPENDENT MECHANISM
“Although the present study and several previous reports suggest that activation of SIRT1 is involved in the muscle sparing effects of resveratrol [9–12], the results reported here do not rule out the possibility that some of the effects of resveratrol were SIRT1-independent. It should be noted that other potential mechanisms that may be involved in the anti-catabolic effects of resveratrol have been described. These mechanisms include antioxidant effects [5,6], inhibition of NF-kB [7] and iNOS activities [8], prevention of insulin resistance [4,45], and increased microvascular recruitment in skeletal muscle [46]. It is of course possible, and perhaps even likely, that several of these mechanisms are interconnected. For example, inhibition of NF-kB by resveratrol may reflect SIRT1-dependent deacetylation of NF-kB/p65 [47] and antioxidant effects may reflect improved PGC-1α-regulated mitochondrial biogenesis [11,42].
Interestingly, a recent study by Centeno-Baez et al [8] suggests that mechanism(s) regulating the anti-catabolic effects of resveratrol may depend on the mediators involved in muscle wasting and that different effects of resveratrol may be regulated by different mechanisms. Thus, in that study [8], treatment of cultured L6 muscle cells with a mixture of TNFα, IFNγ, and LPS resulted in increased iNOS expression and NO levels. These effects of the cytokine/LPS mixture were inhibited by resveratrol in a dose-dependent manner and because the effects of resveratrol were not blocked by different SIRT1 inhibitors, the authors concluded that the beneficial effects of resveratrol did not reflect SIRT1 activation. This conclusion was further supported by the inability of resveratrol to deacetylase PGC-1α in untreated control cells (although the influence of resveratrol on the status of PGC-1α acetylation in cytokine/LPS-treated muscle cells was not reported). In contrast, downregulation of AMPK with siRNA or treatment of the muscle cells with the AMPK inhibitor Compound C blunted the ability of resveratrol to prevent the cytokine/LPS-induced iNOS expression and NO production and the authors concluded that resveratrol inhibition of iNOS in skeletal muscle involves AMPK but not SIRT1 [8]. Although these results suggest that resveratrol targets a different mechanism in muscle cells treated with cytokines and LPS [8] than in muscle cells treated with dexamethasone [present study and ref # 30], the apparently contradictory results may also suggest that resveratrol inhibits the expression of atrogin-1, MuRF1, and UCP3 and the expression of iNOS through different mechanisms.
The present study is important because it provides novel information about the influence of resveratrol on glucocorticoid-induced muscle wasting. In addition, the results provide molecular evidence that the muscle-sparing effects of resveratrol are at least in part regulated by SIRT1 and reflect inhibited upregulation of the ubiquitin ligases atrogin-1 and MuRF1.
Radiation-induced Lumbo-sacral Plexopathy in Cancer Survivors
Radiation-induced lumbo-sacral plexopathy is a chronic handicap, frightening because progressive and usually irreversible, usually appearing several years after radiotherapy
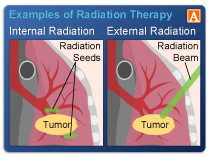
Cancer patients undergo radiation for many reasons. Radiation can cause short, long-term and late stage adverse events. If the radiation damage is severe enough, the cancer survivor can develop Radiaton-Induced Lumbosacral Plexopathy.
When I first presented with pain and nerve damage in my neck (my cancer) in early 1994, my doctors weren’t sure if I had a single bone plasmacytoma (pre-myeloma) or full-blown multiple myeloma. The decision that I had pre-myeloma and therefore not to treat my cancer systemically turned out to be critical to me.
Approximately 10 months after my initial diagnosis and surgery, I developed extensive lesions in my iliac crest. I then underwent aggressive local radiation.
The radiation stopped the bone pain within weeks. However the radiation left me sterile and resulted in radiation damage. Though I didn’t know this at the time, this aggressive radiation therapy led to progressive weakening of my legs. I underwent more radiation in 1996. The long, slow decline of my lower-body muscle and organ function began a few months after my radiation therapy. I am able to walk with difficulty.
If you undergo radiation therapy as cancer therapy for any reason there is a risk of short, long-term and late stage damage. The key is to prevent the damage rather than try to reverse the damage years after the damage has occurred. If your oncologist tells you that the damage caused by radiation is mild and will probably heal someday please be proactive. Take steps to prevent long-term damage.
Needless to say I have a keen interest in the research linked and excerpted below. At this point in my life I have no interest in taking pentoxifylline. The side effects look pretty serious. However I plan to continue researching the issue in hopes of staying out of a wheelchair. It helps to discuss issues in a support group with other RILP survivors- click now for Facebook’s RILP Support Group.”
Recommended Reading:
- Chemotherapy Side Effects, Allergic Reaction, Hypersensitivity and Anaphylaxis?
- Antioxidants During Cancer Treatment- Yes or No?
- Why Cancer Patients Can’t Trust Conventional Cancer Research
Radiation-induced neuropathy in cancer survivors☆
“Radiation-induced peripheral neuropathy is a chronic handicap, frightening because progressive and usually irreversible, usually appearing several years after radiotherapy…
Promising treatments via the antioxidant pathway for radiation-induced fibrosis suggest a way to improve the everyday quality of life of these long-term cancer survivors.”
The radiation-induced fibroatrophic process: therapeutic perspective via the antioxidant pathway
“The radiation-induced fibroatrophic process (RIF) constitutes a late, local and unavoidable sequela to high-dose radiotherapy, traditionally considered irreversible. Today, this process is partly reversible, thanks to recent progress in understanding the physiopathology of the lesions it causes and the results of recent clinical trials using antioxidant therapy…
The efficacy of combined pentoxifylline–tocopherol treatment in superficial RIF was confirmed in a randomised clinical trial, and then in successful phase II trials especially in uterine fibroatrophy and osteoradionecrosis…”