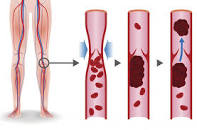
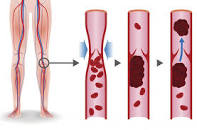
Overall, a substantial risk of VTE associated with lenalidomide-based regimens (MM side effect) was evident in controlled clinical trial settings, despite adequate thromboprophylaxis.”

You’ve been diagnosed with multiple myeloma (MM). You are about to undergo RVd (revlimid, velcade, dexamethasone). Or, your MM has relapsed and your oncologist wants to put you on a chemo combo that includes revlimid (lenalidomide). You are aware of multiple myeloma side effects.
He/she also puts you on a blood clot prophylaxis- this is a fancy word for a therapy that thins your blood to reduce your risk of blood clots.
The problem is, according to the studies linked and excerpted below, blood thinners come with their own risks. Further, even with conventional prophylaxis, revlimid still increases your risk of a blood clot.
What if you could reduce your risk of blood clots (venous thromboembolism) and enhance the efficacy of revlimid/ lenalidomide at the same time?
It is common for oncologists to caution their MM patients about non-conventional nutritional supplementation. I’ve taken omega-3 fatty acids daily for more than 10 years. More importantly, the second study linked below documents the ability of omega-3 to “induce apoptosis’ (fancy expression for “kill MM”) as well as “increased sensitivity to bortezomib in MM cells.”
When I blog about MM, I frequently tell readers that I wish I had known something when I was first diagnosed with MM myself. The ability of omega-3 to kill MM as well as enhance the efficacy of MM to lenalidomide as well as reduce the patients risk of DVT is a perfect example of something I wish I knew back them.

Don’t be surprised or dismayed if your oncologist doesn’t know of the studies linked below. Oncology is based on FDA approved research and therapies so your onc. believes that a blood thinner is therapy enough to reduce your risk of blood clot.
More to the point, your oncologist will be suspect of anything, any therapy that is not FDA approved. Nutritional supplementation like omega-3 fatty acids will never be researched and approved by the FDA.
Your challenge is to read the studies below, email me below if you’d like. and decide for yourself.
To Learn More About Hyperviscosity in Multiple Myeloma- click now
Let me know if you have any questions.
Good luck,
David Emerson
- MM Survivor
- MM Coach
- Director PeopleBeatingCancer
Recommended Reading:
“Patients with multiple myeloma who received lenalidomide-based regimens appeared to have considerable risk for venous thromboembolism, regardless of adequate thromboprophylaxis, according to study results published in Cancer…
“Despite using risk-stratified thromboprophylaxis [for patients with] multiple myeloma receiving lenalidomide [Revlimid, Celgene]-based combination regimens, we still encounter VTE in the clinic, including deep vein thrombosis and pulmonary embolism…”
“Recent observational studies suggest the risk for VTE remains substantial — between 7% and 12% — and that aspirin may not be enough to mitigate VTE risk in some patients with multiple myeloma treated with lenalidomide-based regimens…
“By analyzing evidence from relevant phase 1, 2, and 3 clinical trials identified from Ovid MEDLINE, Embase, and Cochrane databases, researchers estimated the incidence of venous thromboembolism (VTE) among patients with myeloma who have already received thromboprophylaxis with currently used lenalidomide-based regimens.
The included studies were those that assessed lenalidomide-based regimens with thromboprophylaxis.
Overall 1,372 citations were identified, including 51 clinical trials and 9,069 patients examined.
- Aspirin,
- low-molecular-weight heparin or
- warfarin
constituted the most commonly used thromboprophylaxis agents. In trials involving patients who had newly diagnosed and relapsed/refractory myeloma, the pooled incidence of VTE was estimated to be 6.2% over median treatment durations ranging from 2 to 34 cycles, which translated into 1.2 VTE events per 100 patient-cycles.
Overall, a substantial risk of VTE associated with lenalidomide-based regimens was evident in controlled clinical trial settings, despite adequate thromboprophylaxis.”
“Exposure to EPA and DHA induced apoptosis and increased sensitivity to bortezomib in MM cells. Importantly, they did not affect viability of normal human peripheral mononuclear cells…
Our study suggests that EPA and DHA induce selective cytotoxic effects in MM and increase sensitivity to bortezomib and calls for further exploration into a potential application of these n-3 polyunsaturated fatty acids in the therapy of MM.”
Taking blood thinners decreases your risk for blood clots, but it can also increase your risk of heavy bleeding.
If you’re at risk for a heart attack or stroke, blood thinnerscan be lifesaving medications. But they also come with a serious side effect, too: the risk of dangerous heavy bleeding.
Because these meds work by interfering with your blood’s ability to coagulate (clump together), they can either prevent a clot from forming or keep an already-existing one from getting larger. The drawback: If you sustain even a minor injury — say, for example, you cut your finger slicing vegetables — you may have trouble stopping the blood flow.
“Any sort of minor trauma that wouldn’t cause any worry in an otherwise healthy person could be a very serious injury for a patient on a blood thinner,” explains Elliott R. Haut, MD, an associate professor of surgery, anesthesiology, and critical care medicine at Johns Hopkins Medicine in Baltimore. “A minor head injury can be devastating because the body’s normal reaction to stop bleeding doesn’t occur.”