Leave a Comment:
33 comments
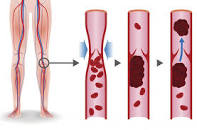
[…] Blood Clots – Myeloma Symptom, Side Effect […]
Reply[…] Myeloma – Symptom, Side Effect – Blood Clots […]
ReplyHi David, i’ve been taking baby aspirin for about 18 months now as directed by my oncologist to prevent blood clotting. I am interested in non-toxic ways to achieve that result. If you could send me the info I would greatly appreciate it. Thank you for the time you invest and all the information you post.
ReplyHi Frank-
I can only tell you what I do to reduce my risk of blood clots. The blog post that you came in on outlines exactly what I do, what I take.
https://peoplebeatingcancer.org/multiple-myeloma-symptom-side-effect-hyperviscosity-blood-clots/
David Emerson
Reply[…] Blood Clots (DVT, hyper-viscosity) […]
Reply[…] Blood Clots (DVT, hyper-viscosity) […]
Reply[…] Blood Clots (DVT, hyper-viscosity) […]
Reply[…] Multiple Myeloma Symptom, Side Effect- Hyperviscosity, Blood Clots… […]
Reply[…] Blood Clots (DVT, hyper-viscosity) […]
Reply[…] Blood Clots (DVT, hyper-viscosity) […]
Reply[…] Blood Clots (DVT, hyper-viscosity) […]
Reply[…] Understanding Blood Clots/VTE and Multiple Myeloma […]
ReplyI started the two weeks ago a few days after finishing radiation. My mo’s nurse practioner told me they wait a month or so after radiation for your body to rest before starting. Then she told me if I would like, I could go ahead and start.
Of course I couldn’t wait to start but now I’m wondering if I should have. I am very tired and achy. It was just my hands and shoulders but today my legs, arms and neck also hurt. After I get up from sitting it’s really bad. It feels like a 2nd day after chemo for me today. I have also been sleeping in and today fell asleep in the chair for more than an hour when the phone rang next to me and woke me. I’m 46 and today I feel like I’m 90.
ReplyHi Emily,
I need more information about your situation before I can offer you some ideas. What did you start? Induction chemotherapy? If so, what is your regimen? Revlimid, Velcade, Dexamethasone (RVd?).
What was the radiation therapy for?
Hang in there,
David Emerson
Reply[…] treatment with melphalan and prednisolone (MP) and radiotherapy (D12-L2 – 30 Gy) were started but suspended after three cycles due to deep venous thrombosis. Partial response was achieved and the patient remained stable until […]
Reply[…] Understanding Blood Clots/VTE and Multiple Myeloma […]
Reply[…] Understanding Blood Clots/VTE and Multiple Myeloma […]
Reply[…] Understanding Blood Clots/VTE and Multiple Myeloma […]
Reply[…] Reading: Green Tea, Curcumin as Integrative, Synergistic Cancer Therapy Understanding Blood Clots/VTE and Multiple Myeloma Deep Vein Thrombosis, Venous Thromboembolism aka Blood Clot in cancer patients and […]
ReplyHi Mena-
I supplement with Wobenzyme N. I have developed two blood clots from chemo and wobenzyme plus nattokinese has helped me resolve the clots.
David
Reply[…] Understanding Blood Clots/VTE and Multiple Myeloma […]
Reply[…] Understanding Blood Clots/VTE and Multiple Myeloma […]
Reply[…] Understanding Blood Clots/VTE and Multiple Myeloma […]
Reply[…] Understanding Blood Clots/VTE and Multiple Myeloma […]
ReplyHello David,
I had DVT at age 45 (in 2001) with no known cause evidenced by multiple blood tests. They did not test for MGUS/MM at that time. I was taking warfarin for about a year since they didn’t find a cause. I was then put on a non-warfarin blood thinner (Plavix) which I took for a few years. A new primary care doctor wanted me to see a hematologist to see if I should be on Plavix since he saw a couple of odd results from a CBC. The hematologist said to go off Plavix but was more concerned because he discovered I had TTP and MGUS. After being off blood thinners altogether for awhile I developed another DVT. I have been taking warfarin ever since — about 7 years.
I’d really like an alternative, and after reading your article, I’m going to discuss with my doctor the possibility of trying the: Wobenzym N, omega 3 fatty acids, and nattokinase supplementation.
I’m wondering which brands you take.
Thank you for your time and this great article.
Diana
ReplyHi Diana,
I understand what you are thinking because I went through something similer. However, when I wrote the post I left out my appoitments with my GP at the time, who had a difficult time with me switching from “standard-of-care” (warfarin) to anything else. In fairness to my PBC, this is the way medicine works in the U.S. The FDA tests and approves therapies that certified medical doctors then prescribe to their patients.
I am curious to see what your doctor says to you about switching from conventional to non-conventional. Let me know if you think of it.
As for brand names of the supplements I take, Wobenzym N is a brand from a company called Wobe Mugos (german I think). I take Life Extension Super Omega 3 and AllergyResearch Group nattokinase.
Good luck,
David Emerson
ReplyI often wonder if I am on warfarin because of MMor because I have an artificial heart valve. In either case can I try the methods you have listed above and be fine.
ReplyBrilliant David! thank you very much. I was diagnosed with MM in 5/2015 and was treated with VTD and Daltaparin blood thinning injections. In 11/2015 I had a STC and went into remission-yay! In 12/2016 I relapsed. I am now on CDT and Daltaparin injections with my next STC planed for 3-4 months time. Can you please give me your expertise on any supplements I need to take or what I can do to assist healing in all of the lesions throughout my face and body. To help kill the cancer cells. Any information will be very gratefully received. Many thanks and congratulations on your continued good health. Kindest regards
ReplyHi Andrina-
There are a number of supplements shown to by cytotoxic to MM and there are also other supplements shown to work synergistically with certain chemotherapy regimens. An example would be thalidomide/revlimid and curcumin.
I will email the integrative therapies guide to your email address. Please consider getting the complete MM cancer coaching package.
Good luck,
David Emerson
Reply[…] Understanding Blood Clots/VTE and Multiple Myeloma […]
Reply