
Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Multiple Myeloma Symptom, Side Effect- Infection
Multiple Myeloma Symptom, Side Effect- Infection
“We show that the risk of infections and infection-related death is significantly increased in MM patients compared to controls.”
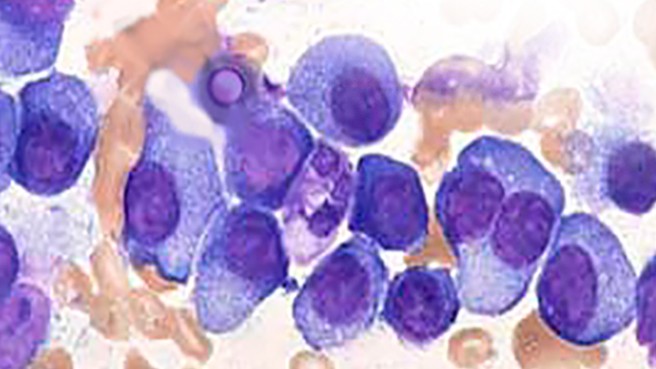
Myelosuppression is the most common cause of death (COD) among multiple myeloma patients. Infection and blood-related COD is both a multiple myeloma symptom and a multiple myeloma side effect.
While the general term myelosuppression speaks to the reduction in any type of blood cell- red, white, platelets- infection comes from reduced white blood cells. That is to say, multiple myeloma (monoclonal proteins) among other things, interfere with the creation of white blood cells that create antibodies. Reduced antibodies makes a person become susceptible to infection.
Multiple myeloma cells can interfere with the creation of white blood cells and chemotherapy and radiation can interfere with the creation of white blood cells.
Infection, or an increased risk of infection, can be caused either/or/both by monoclonal proteins (MM) or chemotherapy/radiation.
Myeloma patients are often diagnosed with anemia caused by myeloma cells crowding out red blood cells. Myeloma patients often develop a side effect from chemotherapy called neutropenia.
The challenge of all MM survivors is to prevent infections caused by your cancer as well as infections caused by the therapies prescribed to manage your cancer.
Problems with the health of your bone marrow due to:
can often be a life and death challenge for the newly diagnosed multiple myeloma patient. According to the research linked below, MM patients can die of infection after weeks, months or years. The research doesn’t specify if the infection is due to problems caused by multiple myeloma (symptoms) or problems caused by chemotherapy or radiation (side effects).
In my experience there are two possible solutions:
- First, evidence-based but non-conventional therapies shown to both prevent damage to blood cells. Nutrition, supplementation and lifestyle therapies shown to enhance the health of red, white blood cells and platelets.
- Secondly, adopt a “less is more” approach to chemotherapy and radiation. Keep in mind that standard-of-care multiple myeloma chemotherapy regimens often call for a high-dose approach to managing cancer. If your oncologists recommends an autologous stem cell transplant, ask him/her to explain the overall survival benefits of this aggressive, expensive, debilitating procedure.
It is important to remember that supplementation has been shown to prevent the long-term bone marrow damage caused by chemotherapy.
To learn more about evidence-based non-conventional therapies to manage your multiple myeloma, scroll down the page, post a question or a comment. I will reply to you ASAP.
- To Learn More About Myeloma Symptoms click now
- To Learn More About What Myeloma Patients Die From- click now
- To Learn More About Inflammation and side effects-click now
- Click now to learn more about thrombocytopenia
- To Go To Multiple Myeloma Explained- click now
Hang in there,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Multiple Myeloma Side Effects- Prevent, Heal Chemobrain
- Bone Imaging Can Make or Break Multiple Myeloma
- Multiple Myeloma Side Effects- Low Neutrophils aka Leukopenia- Help!
Multiple myeloma and infections: a population-based study on 9253 multiple myeloma patients
“In this large population-based study based of over 9000 MM patients diagnosed in the period 1988–2004 with follow up to 2007, and almost 35,000 controls, we show that the risk of infections and infection-related death is significantly increased in MM patients compared to controls. The increase in cumulative incidence was consistently elevated in comparison to controls in all years analyzed, but highest during the first year following diagnosis. We found that the risk of infections has increased in recent years..”
Bone marrow suppression
“Bone marrow suppression also known as myelotoxicity or myelosuppression, is the decrease in production of cells responsible for providing immunity (leukocytes), carrying oxygen (erythrocytes), and/or those responsible for normal blood clotting (thrombocytes).[1] Bone marrow suppression is a serious side effect of chemotherapy..
Nonsteroidal anti-inflammatory drugs (NSAIDs), in some rare instances, may also cause bone marrow suppression..
Many other drugs including common antibiotics may cause bone marrow suppression. Unlike chemotherapy the effects may not be due to direct destruction of stem cells but the results may be equally serious. The treatment may mirror that of chemotherapy-induced myelosuppression or may be to change to an alternate drug or to temporarily suspend treatment…”
How Chemotherapy Affects the Immune System
“Your healthy cells typically can repair the damage from chemotherapy once treatment ends. (One notable exception is nerve cells in your hands and/or feet, which can be permanently damaged by certain chemotherapy medications — a condition known as peripheral neuropathy.)
As chemotherapy medicines damage the bone marrow, the marrow is less able to produce enough red blood cells, white blood cells, and platelets. Typically, the greatest impact is on white blood cells. When you don’t have enough white blood cells, your body is more vulnerable to infection…
Although most chemotherapy medications can have an impact on your immune system, how much of an impact depends on many factors, such as:
- which medicines you’re taking and in what combination — having two or three at once is more likely to affect the immune system than having one
- how much medicine is given and how often medicine is given (dosing)
- how long treatment lasts
- your age and overall health
- other medical conditions you have…
Before, during, and after chemotherapy, do your best to follow the common-sense ways to take care of your immune system, such as getting enough rest, eating a healthy diet, exercising, and reducing stress as much as you can…
Cancer therapy-induced residual bone marrow injury-Mechanisms of induction and implication for therapy
“However, many patients receiving chemotherapy and/or ionizing radiation (IR) also develop residual (or long-term) BM injury (a sustained decrease in HSC reserves due to an impairment in HSC self-renewal) after the recovery from acute myelosuppression.
Unlike acute myelosuppression, residual BM injury is latent and long lasting and shows little tendency for recovery.
Following additional hematopoietic stress such as subsequent cycles of consolidation cancer treatment or autologous BM transplantation, residual BM injury can deteriorate to become a hypoplastic or myelodysplastic syndrome…
The majority of chemotherapeutic agents can cause myelosuppression in a dose-dependent manner. Among these compounds, alkylating agents, pyramidine analogs, anthracyclines, anthraquinones, nitrosoureas, methotrexate, hydroxyurea and mitomycin C are highly cytotoxic to BM [6,7]…
Although many patients recover rapidly from an acute myelosuppression after chemotherapy and/or IR with or without HGF treatment, some will develop residual (or long-term) BM injury manifested by a decrease in HSC reserves and an impairment in HSC self-renewal [6,9,10]…
Unlike acute myelosuppression, residual BM damage is latent. Patients and animals with residual BM injury usually have normal blood cell counts under normal homeostatic conditions in spite of a decrease in HSC reserves [9,10,14].
Because of this latency, the clinical implications of the residual BM injury have been largely overlooked. Moreover, the importance of long-term BM damage is further obscured by the seemingly complete recovery of peripheral blood cell counts, BM cellularity and the number of colony-forming units (CFUs) especially after the use of HGFs.
In fact, the use of HGFs may worsen chemotherapy- and IR-induced residual BM damage by promoting HSC and HPC proliferation and differentiation at the expense of HSC self-renewal [12,15,16].
This could lead to an accelerated exhaustion of HSCs and further compromise the long-term recovery of BM hematopoietic function. Although residual BM damage is latent, it is long lasting and shows little tendency for recovery.
It can lead to the development of hypoplastic marrow or a myelodysplastic syndrome at later times or following additional hematopoietic stress such as subsequent cycles of consolidation cancer treatment or autologus BM transplantation [9,10,14]…
Bone marrow infiltration by multiple myeloma causes anemia by reversible disruption of erythropoiesis
“Multiple myeloma (MM) infiltrates bone marrow and causes anemia by disrupting erythropoiesis, but the effects of marrow infiltration on anemia are difficult to quantify…”

