Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Multiple Myeloma Symptom- SRE aka Bone Damage
Multiple Myeloma Symptom- SRE aka Bone Damage

“Concurrent management of (bone damage) with approved therapies as well as evidence-based management of the MM with the most effective therapies early in the disease life-cycle itself might be the key to management of SREs…”
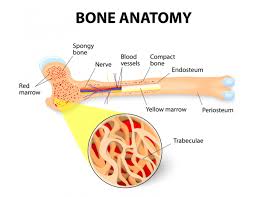
Multiple Myeloma (MM) is considered a blood cancer. However, MM starts in the patient’s bone marrow and eats away at the patient’s bone. This “eating away” causes skeletal-related events aka SREs, aka bone damage. Bone damage is a primary multiple myeloma symptom.
The article linked and excerpted below does an excellent job of outlining the problem of bone damage as a multiple myeloma symptom as well as a complication of a relapse of this disease.
According to the study below, “More than 80% of patients with MM have osteolytic bone disease.”
SRE, Bone damage as multiple myeloma symptom:
Before a person is diagnosed with MM, he/she is likely to experience bone pain. Pain in your spine or hips are common, in my experience. I experienced neck pain during the three months that preceded my own diagnosis of MM. I ignored the pain until it became severe. Big mistake on my part…
SRE, Bone damage as a side effect of therapy:
The challenge that MM patients face is that standard-of-care therapies can cause SRE, bone damage. For example, dexamethasone is known to cause damage to bone health.
Diagnostic testing for SRE, Bone damage:
The bad news is that the threat of SRE/pathological fractures/hypercalcemia to the myeloma patient and/or survivor is ongoing. Your bone health is a priority for the rest of your life.
The good news is that this threat can be diagnosed relatively early before real damage is done. Hypercalcemia can be identified on your blood testing through serum calcium. Pathological fractures can be identified by imaging studies- x-ray, CT, MRI and PET scans.
Bone damage is expensive for the MM patient and bone damage is a a predictor of morbidity, mortality, and decreased quality of life. In short, the MM patient and survivor should do everything in their power to increase their bone health. While bisphophonate therapy is the standard-of-care therapy given to MM patients to harden their bones, this class of chemotherapy comes with it’s own short and long-term side effects.
Evidence-based, non-toxic therapies to strengthen bones are:
More good news. Conventional or traditional oncology versus non-conventional oncology should not be an all-or-nothing kind of thing. In other words, when I was diagnosed with MM, I underwent conventional FDA approved MM therapies and now that I am in remission, I undergo all of the evidence-based non-conventional therapies as well.
Many of the bone strengthening therapies I’ve highlighted are also therapies shown to fight multiple myeloma. The best two examples of this is the supplement called curcumin and vitamin D3. Actually, frequent, moderate exercise is another great example of a therapy shown to fight MM as well as strengthen bones.
My point is that you shouldn’t expect your oncologist to talk up non-conventional therapies. He/she just isn’t trained to promote exercise, supplementation or nutrition and how these therapies effect MM. In addition, you shouldn’t take the fact that conventional oncology does not prescribe non-conventional therapies as proof that these therapies do not work. My MM survival since early 1994 is proof that these therapies work.
SRE’s, bone damage is a key multiple myeloma symptom and side effect. To learn more about evidence-based, non-toxic therapies that promote bone health, scroll down the page, post a question or comment and I’ll reply to you ASAP.
In the meantime, hang in there,
David Emerson
- MM Survivor
- MM Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Multiple Myeloma Diet- Before, During, After Therapy
- Multiple Myeloma, Zoledronic Acid, Renal Dysfunction, Bone Disease
- Multiple Myeloma, Dex, Glucocorticoids, Your Bone Health
Presence of Skeletal-Related Events in Multiple Myeloma More than Double Health Care Costs
“Patients with newly diagnosed multiple myeloma(NDMM) who experience skeletal-related events (SREs) accumulate more than double the all-cause health care costs than matched patients with NDMM without SREs. Furthermore, healthcare costs increase in proportion to the number of SREs. These study findings were published in the Journal of Oncology Pharmacy Practice.
…More than 80% of patients with MM have osteolytic bone disease, which is a predictor of morbidity, mortality, and decreased quality of life.
Skeletal-related events, a complication of osteolytic bone disease, are defined as:
- pathological fractures,
- hypercalcemia, and
- spinal cord compression, and
- undergoing radiation to bone and surgery to bone…
Matching for well-balanced baseline characteristics yielded cohorts of 3432 patients for comparative analysis. From this, results indicated that patients with SREs accrued significantly higher outpatient, inpatient, and pharmacy healthcare resource utilization compared with patients without SREs.
The average annual all-cause health care cost for patients with SREs was $213,361, whereas the cost for patients without SREs was $94,896 (P <.001). At 38.7% of the total cost, hospitalization was the leading driver of increased costs.
Health care costs also increased in proportion to the number of SREs. Across all 6648 patients with SREs, the average annual SRE-related health care costs were:
- $39,603 for patients with 1 SRE;
- $45,463 for those with 2 SREs; and
- $50,111 for those with 3 SREs.
For each group of total number of SREs, inpatient services comprised the majority of the health care expenses.
The authors noted that these results indicate under-utilization of prophylactic treatment of SREs. “Concurrent management of bone complications with approved therapies as well as evidence-based management of the MM with the most effective therapies early in the disease life-cycle itself might be the key to management of SREs in this so far incurable and chronic malignancy,” they concluded.
Reference
Ailawadhi S, Medhekar R, Princic N, et al. Healthcare resource utilization and costs in patients with multiple myeloma with and without skeletal-related events [published online October 20, 2019]. J Oncol Pharm Pract. doi: 10.1177/1078155219881489