Multiple Myeloma stages, symptoms, and prognosis are important first steps for the newly diagnosed myeloma patient. But do not make the mistake of thinking that your fate is set…
Diagnosing and staging multiple myeloma (MM), while important, is perfunctory. A MM patient’s stage at diagnosis is a bunch of numbers. I’ve linked the stages, the diagnostic values, below in the article from cancer.net.
Please do not misunderstand me. I believe it is essential for newly diagnosed patients to receive and accurate diagnosis and stage. My point is that this is the start of your MM experience. That your stage is not your MM fate, as they say.
My problem with conventional oncology is that while the newly diagnosed MM patient may not be able to absorb detailed information about his/her advanced MM, many MM patients are told to begin aggressive therapy immediately.
If an oncologist is going to give patients time to learn about multiple myeloma, they should also give patients time to think about possible therapy plans.
Unpredictability is the hallmark of a multiple myeloma (MM) diagnosis. Even a diagnosis of advanced MM. After studying and coaching multiple myeloma for more than 20 years, I’m more confident talking about side effects than I am about a MM patient’s prognosis.
I reached end-stage MM in September of 1997. My fourth oncologist in four years told me that there was “nothing more that they could do for me.” I understand that my case is an outlyer as MM goes. I began an alternative therapy two months later and achieved complete remission 17 months after that.
My point is that if you recieve a diagnosis of stage III multiple myeloma, take a week or two to think through your options. I think you will appreciate it in the long run.
Have you been diagnosed with advanced multiple myeloma? To learn more about your options, scroll down the page, post a question or comment and I will reply to you ASAP.
Hang in there,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
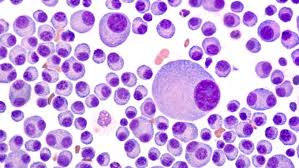
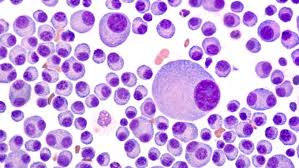
“Staging is a way of describing where a cancer is located, if or where it has spread, and whether it is affecting other parts of the body.
Doctors use diagnostic tests to find out the cancer’s stage, so staging may not be complete until all of the tests are finished. Knowing the stage helps the doctor decide what kind of treatment is best and can help predict a patient’s prognosis, which is the chance of recovery. There are different stage descriptions for different types of cancer…
For myeloma, it is important to begin with whether the patient is experiencing symptoms. It is common to classify people with newly diagnosed myeloma as being either symptomatic from the disease (having symptoms and signs) or asymptomatic (not having any symptoms)…
The symptoms related to myeloma are described with the mnemonic acronym “CRAB,”with each letter corresponding to a symptom:
- Calcium levels are increased, which is known as hypercalcemia. This is defined as a serum calcium level greater than 0.25 mmol/L above the upper limit of normal or a level that is greater than 2.75 mmol/L.
- Renal, or kidney, problems, identified as a creatinine greater than 173 mmol/L.
- Anemia is defined as having a low hemoglobin level, which is 2 g/dL below the lower limit of normal or a hemoglobin level that is less than 10 g/dL.
- Bone pain or lesions include:
- lytic lesions (areas of bone damage)
- osteoporosis (thinning of the bones)
- compression fracture of the spine
“Explaining to a patient that they have stage IV cancer (stage III multiple myeloma) is a difficult scenario, but it should include a candid discussion about life expectancy and treatment efficacy so as not to build false hopes.
Otherwise the patient cannot truly give informed consent to treatment, argues Donald Brand, PhD, adjunct professor at the NYU Long Island School of Medicine and former director of Health Outcomes Research at NYU Winthrop Hospital, New York City.