
Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Myeloma Imaging
Myeloma Imaging
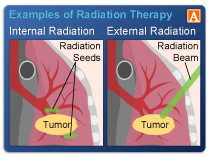
Myeloma imaging tests are the only way I know of to look IN to your bones to see if there is any bone involvement. The challenge is that radiation comes with some forms of imaging.
In the spirit of full disclosure I will admit that I have undergone many different types of imaging tests and I have undergone local radiation to my iliac crest twice as palliative therapy for my multiple myeloma.
I’m cautious about radiation exposure. And I don’t think oncology thinks long-term about the side effects of…anything.
The first study linked and excerpted below explains what I have suspected for years. Even small doses of radiation can cause health problems. Especially to the patient’s heart.
To some degree, myeloma patients are between a rock and a hard place when it comes to imaging diagnostic testing. We need to look in our bones routinely to see if there are any monoclonal proteins growing.
Radiation is cumulative. Every rad increases your risk of DNA damage or a secondary cancer. Over a lifetime of living with myeloma diagnostic testing, your radiation exposure can add up.
Talk with your oncologist about having an MRI instead of a CT the next time he/she wants you to undergo diagnostic imaging.
Do you have multiple myeloma? Consider evidence-based therapies shown to enhance the efficacy of radiation. Scroll down the page, post a question or comment. I will reply to you ASAP.
Thanks,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
New evidence strengthens link between low dose radiation and increased risk of heart disease
“Exposure to low doses of ionizing radiation is associated with a modestly increased excess risk of heart disease, finds an analysis of the latest evidence published by The BMJ today.
The researchers say these findings “have implications for patients who undergo radiation exposure as part of their medical care, as well as policymakers involved in managing radiation risks to radiation workers and the public.”
And a linked editorial suggests that these risks “should now be carefully considered in protection against radiation in medicine and elsewhere.”
It’s well recognized that exposure to high-dose radiation can damage the heart, but firm evidence linking low-dose radiation to heart disease (eg. scatter radiation dose from radiotherapy or working in the nuclear industry) is less clear…
After taking account of other important factors, such as age at exposure, the researchers found consistent evidence for a dose-dependent increase in cardiovascular risks across a broad range of radiation doses…
This equates to a modest but significantly increased excess lifetime risk of 2.3-3.9 cardiovascular deaths per 100 persons exposed to one Gy of radiation, explain the authors…
The authors suggest that mechanisms for these cardiovascular effects are poorly understood, even at high dose…
They also acknowledge that few studies assessed the possible modifying effects of lifestyle and medical risk factors on radiation risk, particularly major modifiable risk factors for cardiovascular disease like smoking, obesity, diabetes, high blood pressure and high cholesterol, and say further research is needed in this area…
Imaging in multiple myeloma: How? When?
“In this review,
- the advantages,
- indications of use,
- and applications of the 3 techniques in the management of patients with MM in different settings will be discussed.
The European Myeloma Network and the European Society for Medical Oncology guidelines have recommended WBLDCT as the imaging modality of choice for the initial assessment of MM-related lytic bone lesions.
Magnetic resonance imaging (MRI) is the gold-standard imaging modality for detection of bone marrow involvement, whereas PET/CT provides valuable prognostic data and is the preferred technique for assessment of response to therapy. Standardization of most of the techniques is ongoing…
Magnetic resonance imaging (MRI) has been established as a valuable technique for diagnosing bone involvement in MM.24 MRI is based on examining the composition of the tissue with regard to water and fat content and has the highest sensitivity when it comes to detecting BM infiltration by myeloma cells, without radiation exposure…
Several studies have shown that MRI, either axial or whole body, is more sensitive than whole-body X-ray for the detection of bone involvement in MM, affording higher diagnostic precision.29,30
Studies that have compared MRI with PET/CT have shown that the 2 techniques are equally effective in detecting FLs.19 Studies comparing MRI with WBLDCT have suggested excellent agreement in terms of lesion detection, pattern, and BM involvement.31 MRI FLs correlate with standard known prognostic factors, in particular cytogenetics, and with clinical outcomes.29,32,33 On the contrary, the prognostic meaning of a diffuse pattern is less clear; addition of the DWI technique as an adjunct may clarify this issue.34 …
When making a choice, one should also remember that findings at baseline impact on interpretation of the same findings after therapy. Because the detection of lytic bone lesions, which are eventually at risk for developing possible complications, is the mainstay for starting anti-MM treatment and managing MM patients correctly…”


