
Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- non-conventional therapies »
- Myeloma, Medical Cannabis & the Patient/Oncologist Relationship
Myeloma, Medical Cannabis & the Patient/Oncologist Relationship
…open and unrestricted communication is vital in preserving the patient-doctor relationship and ensuring proper treatment [11, 13].”
The “Patient-Doctor relationship” is what oncology should be about. In other words, multiple myeloma survivors rely on their oncologists. We look up to our oncologists. We believe everything they say.
In my 25 plus years as a multiple myeloma survivor, I’ve come to believe that “the patient-oncologist relationship” is about oncology’s relationship with the FDA. My experience is that oncologists don’t focus on cancer patients. They focus on what the FDA considers to be legitimite or what the FDA believes is “evidence-based.”
The Ethisist exerpt below from the 2/5/19 NYT Sunday Magazine illustrates what I’m talking about.
How many multiple myeloma patients have asked their oncologists about an evidence-based but non-conventional (not approved by the FDA) therapy and been similarly dissuaded or completely shut down? How many MM patients reading this post have been similarly shut down by their oncologist when asking about diet, nutritional supplementation or some other evidence-based but non-conventional therapy?
Because the patient discussed below is a survivor of my cancer, multiple myeloma (MM) and because I have frequent, ongoing interaction with MM patients and survivors, I have some insight into why patients might want to include medical cannabis in their therapy plan. MM patients who want to include CBD oil believe that it will:
- ease their bone pain,
- reduce their nausea,
- enhance the efficacy of their chemotherapy and
- may even be cytotoxic to their myeloma.
All for a relatively inexpensive, accessable therapy with little if any risk aka side effects.
As for the oncologist’s view point, my guess is that the oncologist referenced below doesn’t want to discuss CBD oil with his/her patient for two reasons:
- The research of medical marijuana and MM is minimal
- CBD oil is not FDA approved
So a patient with an “incurable” blood cancer, multiple myeloma, may want to try CBD oil. However, if an oncologist doesn’t consider the therapy to be evidence-based (clinical trial), then he/she will not consider it. Because there is no real definition of the term evidence-based, it is what the oncologist considers “evidence-based.”
Rather than putting the patient-doctor relationship first by communicating with the patient, the oncolgist simply tells the MM patients that if he uses cannabis he/she will fire the patient. More often than not, simply refusing a patient will force the patient to do what he/she thinks is best and not tell the oncologist. A lose-lose scenario.
Have you been diagnosed with cancer? Scroll down the page, post a question or comment if you would like to learn more about CBD oil and cancer.
Hang in there,
David Emerson
- Multiple Myeloma Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Cannabis as Cancer Therapy-
- Marijuana’s Health Risks and Benefits- Cancer, Heart, Memory, etc.
- $ Taints Oncology Research- Always Has, Always Will-
Can a Doctor Refuse to Treat a Patient Who Takes Cannabis?
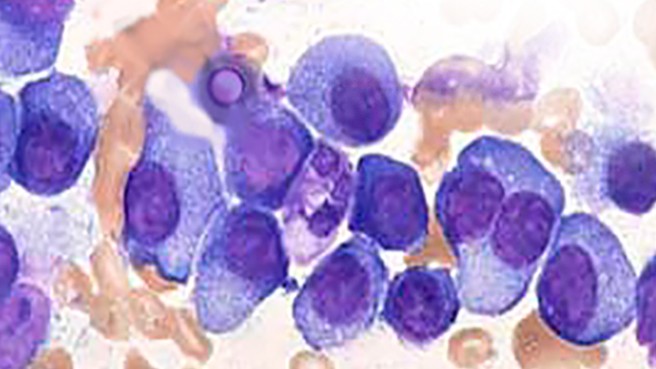
Question: “A friend was recently diagnosed with multiple myeloma, a cancer of a type of white blood cell called plasma cells. There is often significant pain associated with this condition, and my friend has been treated with high doses of different opioid combinations, in addition to chemotherapy. My friend lives in Colorado, where he has easy access to medical marijuana, and he asked his oncologist if he could add this to his regimen in hopes of decreasing his dependence on opioids. The oncologist told him that he would refuse to treat my friend if he took any form of cannabis…
The National Cancer Institute states that cannabis may benefit patients suffering from cancer-related side effects. Cannabis is routinely recommended for cancer patients to improve appetite, decrease nausea and alleviate pain. The medical literature is fairly consistent on the efficacy and minimal side effects of cannabis, which has specifically been shown to help patients decrease opioid dependence. There are even some reports that cannabis may be a valuable adjunct to chemotherapy in cancer patients.
Is it ethical for the physician to deny treatment based on my friend’s taking cannabis? Is it ethical for my friend not to inform his oncologist if he chooses to use cannabis?
Answer: If it’s just that he disapproves of legal marijuana use, that’s an abuse of the doctor-patient relationship. Patients aren’t obliged to help their doctors enforce a tyrannical demand, so there would be no moral reason your friend should inform him of his cannabis use. Indeed, your friend might want to consider filing a complaint against the oncologist for making this threat…
Physicians, Medical Marijuana, and the Law
“The video showed the boy receiving a marijuana concentrate (oil) which seemed to alleviate his seizures [1]. The oil was high in cannabidiol (CBD), the therapeutic agent in marijuana, rather than delta-9-tetrahydrocannabinol (THC), the psychoactive agent that produces the “high,” so the oil could be used therapeutically while intoxicating the user no more than the medications Charlotte had already tried [1, 2]…
Concerns about Medicinal Marijuana’s Status
Currently, it is illegal for physicians (even in states where medicinal marijuana is legal) to prescribe the drug because it is schedule 1, and prescribing it would constitute aiding and abetting the acquisition of marijuana, which could result in revocation of DEA licensure and even prison time [11].
However, in states where medicinal marijuana is legal, doctors can write a recommendation for the plant, after determining and certifying that the patient suffers from one of the conditions that the state’s law deems to warrant medicinal marijuana [11]—generally debilitating conditions such as cancer, glaucoma, multiple sclerosis, and HIV/AIDS [12].
This recommendation “loophole” was upheld by the US Court of Appeals for the Ninth Circuit in Conant v. Walters, which decided that a physician’s discussing the potential benefits of medicinal marijuana and making such recommendations constitute protected speech under the First Amendment [13]. The court reasoned that doctors should not be held liable for conduct that patients might engage in after leaving the office and that open and unrestricted communication is vital in preserving the patient-doctor relationship and ensuring proper treatment [11, 13].



