
Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Myeloma Patient Experience- The good, the bad, the ugly
Myeloma Patient Experience- The good, the bad, the ugly
“Hello David! I wish we would have found PeopleBeatingCancer.org in 2016 when my 47-yr old husband was diagnosed with Multiple Myeloma.”
Turns out a myeloma diagnosis was only the beginning of my husband’s challenges.
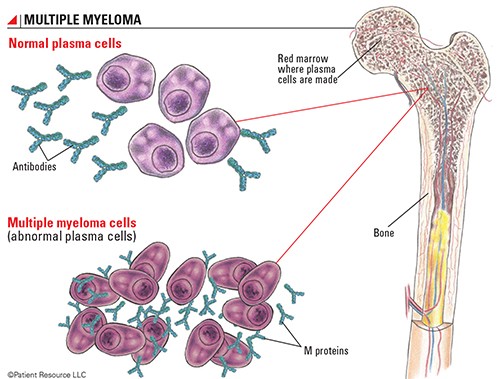
He had emergency surgery for a crushed T-11 vertebra and found two other lesions in his femur and sternum. M-protein (m-spike) was around 3.0. That was 6 years ago. We were scared and followed the conventional protocol, while augmenting with other therapies.
We are a family who HATES pharmaceuticals, don’t smoke, and rarely drink alcohol. We exercise, eats organic foods & juices, carefully read food labels to avoid chemicals, and yet there we were wondering how this could happen.
While my husband learned to walk again, they had him on Revlimid, Velcade, dexamethasone (RVd induction) and radiation treatments. Also, he when to a naturopath for
- high-dose IV Vitamin C,
- IV Curcumin,
- IV Artesunate,
- Mistletoe injections,
- and hydrotherapy,
which cost $25,000 that year.
My husband’s M-protein dropped to 1.0, but the doctors strongly recommended an Autologous Stem Cell Transplant (ASCT) . Since there was this thought of complete remission, we pushed forward.
The stem cell transplant was BURTAL. Harvesting the stem cells prior to the transplant was SO painful. My husband will never do another one again and he is someone who has a high threshold for pain.
His M-protein after the ASCT was 0.7, so it wasn’t much improvement. Also, the radiation was a BIG mistake as he still has pain from those treatments. He also will not do a bone marrow biopsy (BMB) again. He got talked into that the first week and it was not worth the excruciating pain.
The conventional medical cost that year was $500,000, which felt like a money grab by the medical establishment… but again we were fearful and overwhelmed.
After the ASCT, I had my husband go off all conventional therapies so he could recover and try to reverse the neuropathy in his feet, which did improve, but comes back when he goes back on chemo. Seriously, we ALL needed a break from Dexamethasone!
Now he used CBD-THC to help him sleep and it is very effective. The roller-coaster never lets us off. I’ve lost count of the number of times my husband had to go back on conventional therapies. Year 2020 was Daratumumab year.
My husband’s M-protein had decreased to 0.6, but never stays there for long. Currently, he is on Ninlaro and some supplements I found, which are providing improved energy and may possibly be keeping the M-protein holding at 1.0. Seem like when it goes above that mark, he gets bone pain.
I share all these details here so that others may read my story and understand that the information and perspective you share on your website is honest and real. MM patients MUST take charge of their treatment and have some kind of quality of life.
I have met 3 other people with MM and they have all passed on. One I know for sure could have lived longer, but died from the aggressive chemo. I keep looking for other non-conventional treatments that can help keep MM at bay. After all these years, I think it would be nice to be part of a MM community who is actively seeking all kinds of solutions for this illness.
Hi,
Thank you very much for your post. My guess is that your husband was stage III (advanced) when he was first diagnosed with MM. I say this based on his m-spike and extensive bone involvement. On the one hand, it is one of conventional oncology’s greatest accomplishments that a MM patient like your husband can be stabilized.
On the other hand, I agree with you. By undergoing an ASCT, your husband sustained a great deal of toxicity that did little, if anything for his overall survival (OS- length-of-life) and certainly damaged his quality-of-life.
Your comment that your husband’s MM is controlled but never achieves complete remission “but never stays there for long” suggests the control side of the debate below. Consider undergoing just enough chemotherapy to push his numbers back down.
You and your husband learned through painful experience that the “one-size-fits-all” aggressive, curative approach to the MM standard-of-care therapy presents real challenges to the newly diagnosed MM patient and caregiver.
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading-
The PeopleBeatingCancer Side Effects Program
Treatment of Myeloma: Cure vs Control
“Although not often openly acknowledged, “cure vs control” is the dominant philosophical difference behind many of the strategies, trials, and debates related to the management of myeloma. Should we treat patients with myeloma with multidrug, multitransplant combinations with the goal of potentially curing a subset of patients, recognizing that the risk of adverse events and effect on quality of life will be substantial?
Or should we address myeloma as a chronic incurable condition with the goal of disease control, using the least toxic regimens, emphasizing a balance between efficacy and quality of life, and reserving more aggressive therapy for later?
To be sure, if cure were known to be possible (with a reasonable probability) in myeloma, it would undoubtedly be the preferred therapeutic goal of most patients and physicians. But this is not the case. Myeloma is generally not considered a curable disease; however, new definitions of cure have been suggested, including operational cure, which is defined as a sustained complete response (CR) for a prolonged period.1,2 Cure vs control is debated because the strategies currently being tested are not truly curative but rather are intended to maximize response rates in the hope that they will translate into an operational cure for a subset of patients…
In the 1990s, high-dose therapy with autologous stem cell transplant (ASCT) became part of standard practice when it was found to prolong survival compared with conventional chemotherapy.5–7Subsequently, bisphosphonates were found to be effective in decreasing the incidence of bone lesions.8,9
In the past decade, thalidomide,10 bortezomib,11–13 and lenalidomide14,15 emerged as effective agents for the treatment of myeloma, producing spectacular results in combination with other known agents in terms of response rate, CR rate, progression-free survival (PFS), and (more recently) overall survival.
Numerous combinations have been developed, resulting in a veritable alphabet soup of clinical trials,16 and drug combinations are vying with each other for the highest response rate (and prominence).17,18 The results obtained with new combinations have indeed been remarkable and have prompted a relatively new philosophy of treating myeloma with the goal of potential cure rather than disease control. These philosophical differences underpin the various clinically relevant debates regarding myeloma currently confronting patients and physicians.
In fact, it is not uncommon to find that well-meaning investigators interpret the same clinical trial data in opposite ways because they ascribe to different philosophies (cure vs control).19 Although this commentary focuses on myeloma, the cure-vs-control debate may be relevant to other similar chronic malignant and nonmalignant disorders.20–28″

