Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Myeloma Risk Mortality w/ Community Oncologist, Benefit at High-Volume Centers
Myeloma Risk Mortality w/ Community Oncologist, Benefit at High-Volume Centers

“(MM) patients treated by community oncologists had a higher risk for mortality regardless of patient-sharing compared with patients treated by myeloma specialists.”
This post is not a criticism of community oncologists. The study linked below is not saying that community oncologists who treat patients with multiple myeloma (MM) are somehow worse or less skilled than oncologists who practice as “high-volume” centers. I consider this post to be a statement of conventional oncology-at least when it comes to multiple myeloma.
Allow me to us me as a case study.
When I was diagnosed with MM in 2/94 I was treated- surgery, radiation (x3), induction (x5), consolidation (x2) and an autologous stem cell transplant (x1) all at the same hospital. The team of health providers included a general oncologist, surgeon, radiation oncologist, SCT specialist, pathologists, nurses, etc.
University Hospitals of Cleveland is one of the finest hospitals in the country if not the entire world. And we’re talking about MM treatment from ’94-’97- modern times.
After years of studying multiple myeloma treatment, as well as my own case medical file, I can say without prejudice or malice that U.H. made several major mistakes during my treatment- specifically during the first year of my MM experience. Mistakes that led to my oncologist telling me “there is nothing more we can do for you” and diagnosing me as end-stage MM. Again, I am not being critical, I am simply stating facts.
My point is that no one on my team at U.H. specialized in the treatment of multiple myeloma. They just didn’t handle the number of MM cases that “high-volume centers” handle.
The most prominent example of what I’m saying was my original diagnosis of a single plasmacytoma. The original pathologist who tested the plasmacytoma that was removed from my neck diagnosed multiple myeloma not a single plasmacytoma. My general oncologist overruled this diagnosis.
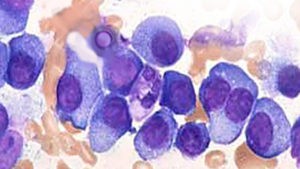
Bone marrow biopsy after BMB failed to identify any abnormal blood work. My team had rarely if ever seen non-secretory multiple myeloma.
These two decisions are clear indications of the limitations of low-volume myeloma treatment versus high-volume centers or MM specialists.
If you have been diagnosed with multiple myeloma consider at least consulting with a MM specialist and consider having major treatments at high-volume centers.
If you’re wondering how/why I’m writing this blog post after being told I was end-stage, I continued my MM therapy at the BRI and achieved complete remission 17 months after my “quack” therapy began on 11/3/97.
Thanks,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Side-Effects Change Multiple Myeloma Patient Decision-Making…
- Resolve Blood Clots (VTE) in Multiple Myeloma (MM)-
- Darzelex + VRd @ Induction Increases sCR, MRD for Multiple Myeloma-
Patients With Myeloma Benefited From Care at High-Volume Centers
Patients with multiple myeloma can benefit from treatment at a high-volume center, according to a new study published in the Journal of the National Comprehensive Cancer Network.
“Our study builds on these data by introducing 2 novel variables — provider volume and patient-sharing — to better understand the impact of individual provider experience and collaboration between multiple specialists and community oncologists,” the researchers wrote.
The researchers gathered data from a state cancer registry linked to public and private health insurance claims to identify a cohort of patients diagnosed with multiple myeloma from 2006 to 2012. They identified 1029 patients. They wanted to see how 3 factors affected overall survival.
The first factor was evaluation at an National Cancer Institute (NCI)-designated Comprehensive Cancer Center (NCICCC). Those patients who were not evaluated at 1 of these centers had a 50% increased risk for mortality compared with patients who received care at these centers (hazard ratio (HR), 1.50; 95% CI, 1.21-1.86; P <.001).
The second factor was outcomes according to the primary oncologists’ volume of patients with myeloma. Those patients treated by low-volume community providers (HR, 1.47; 95% CI, 1.14-1.90; P <.01) and high-volume community providers (HR, 1.29; 95% CI, 1.04-1.61) had significantly higher risk for mortality compared with patients treated by NCICCC specialists. However, no difference was seen in patients treated by NCICCC myeloma specialists and those treated by the highest-volume community oncologists.
“It is possible that survival for patients treated by the highest-volume community providers (eg, ninth and tenth deciles of volume) would be similar to that for patients treated by NCICCC multiple myeloma specialists,” the researchers wrote.
Finally, the researchers looked at outcomes according to patient-sharing between myeloma specialists and community oncologists.
“Because it is not feasible for all patients with multiple myeloma to be treated at an NCICCC, a common practice among community oncologists is to refer a patient to an multiple myeloma specialist for initial treatment recommendations or transplant evaluation, but to perform most care in the community,” the researchers wrote.
Again, patients treated by community oncologists had a higher risk for mortality regardless of patient-sharing compared with patients treated by myeloma specialists.
Reference
Freeman AT, Kuo M, Zhou L, et al. Influence of treating facility, provider volume, and patient-sharing on survival of patients with multiple myeloma. J Natl Compr Canc Netw.2019;17(9):10.6004/jnccn.2019.7298.