“Conclusions: Denosumab combined with risk factors such as dental extraction, poor oral hygiene, use of removable apparatus, and chemotherapy may favor the development of ONJ.”

Osteonecrosis of the jaw (ONJ) is a side effect of the standard-of-care therapy for multiple myeloma (MM), that is approved by the FDA as “safe and effective-” either bisphophonates (zometa, aredia, pamidronate, etc) or denosumab.
The occurrence of this side effect, according to research, is about 2-4%. Both types of therapies can cause ONJ. Though that percentage doesn’t rise to the level of concern, for me at least, what does concern me is that multiple myeloma is a bone disease.
According to the third study linked and excerpted below,
- bisphophonates,
- medical treatments such as radiation and chemotherapy
- steroids such as dexamethasone and prednisone, and
- blood clots and inflammation- both common among MM patients
all can reduce blood flow to bones thereby causeing damage to bones. And it is damage to bones that we MM survivors are specifically trying to avoid!!!
Proposed solutions to bone damage?
- Undergo as little of the offending therapies as possible- Less is More…
- Consider the two evidence-based but non-conventional therapies linked below- either/or/both HBOT or Ozone Therapy to enhance your bone health.
- And finally, consider those bone health therapies outlined in the MM CC Bone Health Guide including nutritional supplementation, nutrition, and lifestyle therapies.
My point is that conventional MM therapies are double-edged swords. Steroids for example, are a chemotherapy adjunct because they have been shown to enhance the efficacy of that chemo regimen. The flip-side of the sword is steroids cause all manner of problems and should be used in moderation.
Are you experiencing bone pain in your joints or in your jaw? Scroll down and post a question or a comment and I will reply to you ASAP.
Hang in there,
David Emerson
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
“Objectives: The aims of this meta-analysis were (i) to perform a systematic review of the relation between treatment with denosumab and the incidence of osteonecrosis of the jaw (ONJ) and (ii) to obtain information on dosage, first event apparition, and treatment approaches for patients with ONJ related to denosumab…
Results: A total of 8963 patients with a variety of solid tumors reported in seven randomized controlled trials (RCTs) were included in the systematic analysis. The overall incidence of ONJ in patients with cancer receiving denosumab was 1.7% [95% CI: 0.9-3.1%]. The use of denosumab was associated with a significantly increased risk of ONJ in comparison with bisphosphonates (BPs)/placebo treatment (RR 1.61, 95% CI: 1.05-2.48, P = 0.029). Subgroup analysis based on controlled therapies demonstrated an increased risk of ONJ in denosumab therapy, when compared with BPs (RR 1.48, 95% CI: 0.96-2.29, P = 0.078) or placebo (RR 16.28, 95% CI: 1.68-158.05, P = 0.017). Similar results were observed for prostate cancer (RR 3.358, 95% CI: 1.573-7.166, P = 0.002).
Conclusions: Denosumab combined with risk factors such as dental extraction, poor oral hygiene, use of removable apparatus, and chemotherapy may favor the development of ONJ.
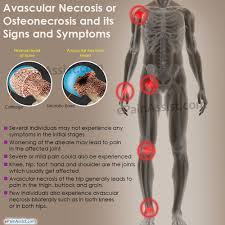
“Avascular necrosis (AVN) is the death of bone tissue due to a loss of blood supply. You might also hear it called osteonecrosis, aseptic necrosis, or ischemic bone necrosis.
If it isn’t treated, AVN can cause the bone to collapse. AVN most often affects your hip. Other possible sites are the shoulder, knees, and ankles…
Causes and Risk Factors for Avascular Necrosis
Things that can make avascular necrosis more likely include:
- Bisphosphonates. These medications that boost bone density could lead to osteonecrosis of the jaw. This could be more likely if you’re taking them for multiple myeloma or metastatic breast cancer.
- Medical treatments. Radiation therapy for cancer can weaken bones. Other conditions linked to AVN include organ transplants, like kidney transplants.
- Steroid drugs. Long-term use of these inflammation-fighting drugs, either by mouth or in a vein, leads to 35% of all cases of nontraumatic AVN. Doctors don’t know why, but longtime use of medications like prednisone can lead to AVN. They think the meds can raise fat levels in your blood, which lowers blood flow.
- Blood clots, inflammation, and damage to your arteries. All of these can block blood flow to your bones.
“All patients symptomatic for MM were also treated with chemotherapy, 3 are women and 1 man, aged 61, 62, 69 and 79. Two patients are IgG, 1 IgA, 1 light chain MM. Three patients have received Zoledronate and 1 Pamidronate followed by Zoledronate for a median time of 19 months (range 6–27). One patient had a wide bone exposition with oro-sinusal fistula, 3 had difficult healing after teeth extractions or oral cleaning. Osteonecrosis of the jaw was histologically confirmed in 1 patient. Patients were treated with antibiotic therapy, underwent surgery (1 emimaxillectomy, 1 curettage, 1 tooth extraction and 1 extraction plus curettage) and local ozone applications according to the schedule. All patients obtained a complete resolution of the problem with the total riepithelialization of the lesions. These preliminary results add further evidence that ozone therapy, with its antimicrobic action and neoangiogenetic properties, results in an improved tissue oxygenation making healing easier…”
“Key message- Hyperbaric oxygen treatment (HBOT) has been suggested as an alternative or adjunct treatment that can prevent further development of osteonecrosis, a bone disease in which bone structure deteriorates. Patients receiving HBOT breathe pure oxygen in a high-pressure chamber. We have summarized research on the clinical effect and safety of HBOT as a treatment for osteonecrosis. We have also examined the cost-effectiveness and budget consequences of HBOT.
- We found two systematic reviews and two randomised controlled trials (RCT) on the effect and safety of HBOT for osteonecrosis, and 13 case studies of safety.
- HBOT can increase the number of patients with osteoradionecrosis of the jaw who achieve full mucosal coverage of the jaw bone.
- It is unclear whether HBOT is more effective than standard treatment results in complete healing of osteoradionecrosis, healing of medication-related osteonecrosis, or a variety of outcomes for ideopathic osteonecrosis of the femur head.
- HBOT-related adverse events appear to be few and transitory…
Background-Osteonecrosis is a bone disease caused by restricted blood supply to the bone tissue in one or more joints. Without adequate blood supply, the body will not be able to form new bone when old bone tissue dies. If this process continues without treatment, bone structure can collapse. Osteonecrosis is most common in the femoral head in the hip joint but may also occur in the shoulder, knee, ankle, hand, foot and jaw.
Osteonecrosis may occur spontaneously, without known cause (idiopathic osteonecrosis), as a complication of, for example, drug use, radiation therapy, high alcohol consumption or disease (secondary osteonecrosis) or following an injury (traumatic osteonecrosis)…