
Recently Diagnosed or Relapsed? Stop Looking For a Miracle Cure, and Use Evidence-Based Therapies To Enhance Your Treatment and Prolong Your Remission
Multiple Myeloma an incurable disease, but I have spent the last 25 years in remission using a blend of conventional oncology and evidence-based nutrition, supplementation, and lifestyle therapies from peer-reviewed studies that your oncologist probably hasn't told you about.
Click the orange button to the right to learn more about what you can start doing today.
- You are here:
- Home »
- Blog »
- Multiple Myeloma »
- Myeloma, stage 3 young…
Myeloma, stage 3 young…
“In newly diagnosed patients treated with induction, stem cell transplantation, and Revlimid maintenance therapy, the proportion of patients who get to a complete response is approximately 30%
Hi David. I am a newly diagnosed multiple myeloma stage 3 young patient. I am ISS stage 3 , FISH test standard risk with no genetic abnormalities, lesions in spine, and pelvic bone is missing.
I began standard induction therapy of Velcade, Thalidomide, Dexamethasone (VTD).
Over the past two months my blood protein has decreased from 140 to 70 and M-spike or monoclonal protein has decreased from 5.8 g/dl to 0.48 g/dl.
I discontinued the Thalidomide midway because of blood clotting in my hands and feet.
I am 37. Do you think I can be helped? I am from Poland and afraid many thing you might recommended I might not be able to find. Roger
Multiple Myeloma – Stage 3
Hi Roger,
- First, you have stabilized your stage 3 MM. You achieved what is called a Very Good Partial Remission (VGPR).
- Secondly, you have exposed your body to minimal toxicity. If your oncologist had his/her way (probably) you would undergo several more rounds of therapy in hopes of achieving complete remission (CR).
- MM Survivor
- MM Cancer Coach
- Director PeopleBeatingCancer
Recommended Reading:
- Velcade/Bortezomib- CIPN, Heart, Blood, Muscle Damage
- Stem Cell Transplant- Treatment-related Secondary Cancer
- Multiple Myeloma Chemotherapy = Accelerated Aging
To be sure, if cure were known to be possible (with a reasonable probability) in myeloma, it would undoubtedly be the preferred therapeutic goal of most patients and physicians. But this is not the case. Myeloma is generally not considered a curable disease; however, new definitions of cure have been suggested, including operational cure, which is defined as a sustained complete response (CR) for a prolonged period.1,2 Cure vs control is debated because the strategies currently being tested are not truly curative but rather are intended to maximize response rates in the hope that they will translate into an operational cure for a subset of patients…”
Functional Cure, Defined As PFS of More Than 7 Years, Is Achieved in 9% of Myeloma Patients in the Era of Conventional Chemotherapy and of First-Generation Novel Anti-Myeloma Agents; A Single-Center Experience over 20-Year Period
“Between January 1994 and December 2010, 406 consecutive newly diagnosed MM patients (I am a newly diagnosed multiple myeloma stage 3 young patient) received first line therapy in the Department of Clinical Therapeutics (Athens, Greece).
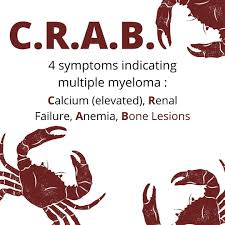
All patients had symptomatic disease, based on the IMWG criteria of that period (at least one CRAB symptom to start anti-myeloma therapy). Thirty-six (8.8%; 23M/13F) patients achieved a PFS of at least 7 years (long PFS group) after frontline treatment.
The median PFS of these 36 patients is 10 years, while the other patients had a median PFS of 22 months…
In conclusion, our study in an unselected group of patients, the majority of whom did not participate in clinical trials, showed that 9% of patients with newly diagnosed myeloma experience prolonged PFS of more than 7 years (median: 10 years) even in the era of CC or first-generation novel agents.
These patients have:
-
- low risk disease,
- ma
- ieve deep responses after ASCT
Long-term health impacts of hematopoietic stem cell transplantation inform recommendations for follow-up
“However, hematopoietic stem cell transplantation (HSCT) survivors are at risk of developing long-term complications, such as
-
-
- endocrinopathies,
- musculoskeletal disorders,
- cardiopulmonary compromise and
- subsequent malignancies.
-
These complications have a direct impact on the morbidity and mortality experienced by HSCT survivors. Two-thirds of HSCT survivors develop at least one chronic health condition; while a fifth develop severe or life-threatening conditions. HSCT patients who have survived for at least 5 years post-transplantation are at a fourfold to ninefold increased risk of late mortality for as long as 30 years from HSCT, producing an estimated 30% lower life expectancy compared with the general population…
No Association Between Response Rates and Survival in Newly Diagnosed Multiple Myeloma
“There was no association between conventional response outcomes, such as CR or VGPR, and survival in patients with newly diagnosed multiple myeloma, according to the results of a meta-regression analysis published recently in the European Journal of Hematology…
“We explored the relationship between response to initial treatment and survival in patients with newly diagnosed multiple myeloma, based on data from 63 randomized clinical trials”…
“Meta-regression analyses failed to demonstrate any association between CR or VGPR with either overall survival or progression-free survival both in patients receiving autologous stem cell transplant [ASCT] and in non-ASCT patients.”
Should Myeloma Patients Panic If They Do Not Achieve A Complete Response?
“Of course, the cause of my worry is not that patients (especially stage 3 patients) have not achieved the magical CR or minimal residual disease-negative status, but at how misinterpretation of data can lead to needless concern, unnecessary chemotherapy increased side effects and cost of care, and even harm…
In newly diagnosed patients treated with induction, stem cell transplantation, and Revlimid maintenance therapy, the proportion of patients who get to a complete response is approximately 30 percent. Does this mean that 70 percent of myeloma patients have “failed”?
Even with more expensive triplet induction regimens such as Revlimid, Velcade, and dexamethasone(Decadron) (abbreviated as RVD), only 40 percent of newly diagnosed myeloma patients achieve complete response. An aggressive seven-drug induction regimen followed by two back-to-back transplants, and three years of maintenance used in the “Total Therapy 3” regimen results in a complete response rate of 55 percent.
Should one-half of newly diagnosed myeloma patients panic that they have not reached a complete response? That would be over 10,000 worried patients each year in the United States alone. The short answer is no; absolutely not.
Multiple myeloma is a remarkably heterogeneous disease; the outcomes vary dramatically depending on the patient’s chromosomal abnormalities. The type of myeloma one patient has may be completely different than the myeloma another patient has; it may not even be the same disease…”
- ISS-1 or -2,
- no high-risk cytogenetics,
- no or mild renal impairment,
- and ach


