According to the research below, your exhaustion and bone pain are common symptoms of MM. Unfortunately, anemia and bone pain are also health problems caused by MM therapies.
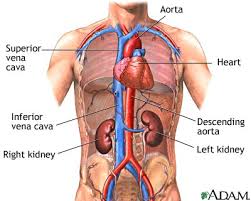
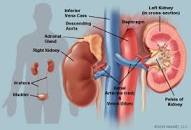
Certain symptoms however, such as renal involvement, can have serious consequences regarding your prognosis and overall survival. It’s in your best interest to understand all you can about any renal damage at diagnosis and the health of your kidney now and in the future.
When you read the information below, try to keep a sharp eye out for symptoms that you experienced that can effect you for years if not the rest of your life.
Most of us MM patients learn about CRAB symptoms. But the article linked below presents more detail for MM patients to learn and remember to help them when considering their therapy plan.
Have you been diagnosed with multiple myeloma? What symptoms have you experienced? To learn more about conventional and evidence-based non-conventional MM therapies, scroll down the page, post a question or comment and I will reply to you ASAP.
Spectrum of disease — Most patients with MM present with signs or symptoms related to the infiltration of plasma cells into the bone or other organs or to kidney damage from excess light chains.
As an example, a retrospective analysis of 1027 sequential patients diagnosed with MM at a single institution found the following symptoms and signs at presentation [10]:
●Anemia – 73 percent
●Bone pain – 58 percent
●Elevated creatinine – 48 percent
●Fatigue/generalized weakness – 32 percent
●Hypercalcemia – 28 percent
●Weight loss – 24 percent, one-half of whom had lost ≥9 kg
Anemia — A normocytic, normochromic anemia (hemoglobin ≤12
g/dL) is present in 73 percent at diagnosis and in 97 percent at some time during the course of the disease [
10]. This anemia can be related to bone marrow replacement, kidney damage,
and/or can be due to dilution in the case of a large M-protein. Anemia commonly results in complaints of fatigue and pallor seen on physical examination.
Macrocytosis (mean corpuscular volume [MCV] >100 fL) was present in 9 percent of 1027 patients studied [
10]. In this study, 53 patients (11 percent) with an MCV >100 fL had a vitamin B12 level <200
ng/L. This finding is similar to a prevalence of vitamin B12 deficiency of 14 percent seen in a separate study of 664 consecutive patients with plasma cell dyscrasias [
31]. While the mechanism for low vitamin B12 levels in these patients is not known, investigations must be done to rule out pernicious anemia.
Bone pain — Bone pain, particularly in the back or chest, and less often in the extremities, is present at the time of diagnosis in approximately 60 percent of patients [
10]. The pain is usually induced by movement and does not occur at night except with change of position. The patient’s height may be reduced by several inches because of vertebral collapse. Plasmacytomas of the ribs occur and can present either as expanding costal lesions or soft tissue masses.
Renal disease — The serum creatinine concentration is increased in almost one-half of patients at diagnosis (and is >2
mg/dL [177
micromol/L] in approximately 20 percent); renal failure may be the presenting manifestation of MM [
10,32]. Two major causes of renal insufficiency in patients with MM are light chain cast nephropathy (also called myeloma kidney) and hypercalcemia. Patients who do not secrete light chains are not at risk for myeloma kidney. In the absence of other causes of renal failure, a presumptive diagnosis of light chain cast nephropathy can be made in the setting of high involved free light chain (FLC) levels (typically >1500
mg/L).
Neurologic disease — Radiculopathy, usually in the thoracic or lumbosacral area, is the most common neurologic complication of MM. It can result from compression of the nerve by a paravertebral plasmacytoma or rarely by the collapsed bone itself.
Cord compression – Spinal cord compression from an extramedullary plasmacytoma (
image 2) or a bone fragment due to fracture of a vertebral body (
image 3) occurs in approximately 5 percent of patients; it should be suspected in patients presenting with severe back pain along with weakness or paresthesias of the lower extremities, or bladder or bowel dysfunction or incontinence.
Central nervous system (CNS) involvement – Intracranial plasmacytomas are rare and almost always represent extensions of myelomatous lesions of the skull or plasmacytomas involving the clivus or base of the skull. Leptomeningeal myelomatosis along with abnormal cerebrospinal fluid findings is uncommon but is being recognized more frequently, especially in advanced stages of the disease [
39-44]. When found it denotes a poor prognosis with survival historically measured in months despite treatment [
43]. It is usually associated with high-risk cytogenetics; lactate dehydrogenase (LDH) levels may be elevated. Survival appears to have improved slightly since the incorporation of immunomodulatory drugs and proteasome inhibitors into first-line therapy [
45,46].
Rare cases of encephalopathy due to hyperviscosity or high blood levels of ammonia, in the absence of liver involvement, have been reported [
47-50]. Myeloma cell lines developed from such patients produce elevated amounts of ammonia, although the mechanism is unclear [
51]. Ammonia levels and the patient’s state of consciousness return to normal if and when the underlying myeloma responds to chemotherapy.
Infection — Patients with MM are at increased risk for infection due to a combination of immune dysfunction and physical factors. Immune dysfunction results from impaired lymphocyte function, suppression of normal plasma cell function, and hypogammaglobulinemia. Physical factors include hypoventilation secondary to pathologic fractures and pain involving the rib cage and spine. Streptococcus pneumoniae and gram-negative organisms are the most frequent pathogens.”